Neonatal Quality Improvement 4
Session: Neonatal Quality Improvement 4
499 - A Quality Improvement Initiative Reduced Methicillin-Susceptible Staphylococcus aureus Infections in a Level IV Neonatal Intensive Care Unit
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 499.3811
Gisel Rivera, Weill Cornell, New York, NY, United States; Jean-Marie Cannon, NewYork-Presbyterian Komansky Children’s Hospital, New York, NY, United States; Kara Mitchell, Wadsworth Center/NYSDOH, Albany, NY, United States; Vivien yap, Weill Cornell Medicine, New York, NY, United States; Katherine Lim, Weill Cornell Medicine, New York, NY, United States; Lars Westblade, Weill Cornell Medicine, New York, NY, United States; Jamie Marino, Weill Cornell Medicine, New York, NY, United States; Priyanka Tiwari, Weill Cornell Medicine, New York, NY, United States; Karen Acker, Weill Cornell Medicine, New York, NY, United States; Liana Senaldi, Weill Cornell Medicine, New York, NY, United States

Gisel Rivera, MD (she/her/hers)
Fellow
Weill Cornell
New York, New York, United States
Presenting Author(s)
Background: Methicillin susceptible Staphylococcus aureus (MSSA) infections are a growing concern in the neonatal intensive care unit (NICU), accounting for 2.6 times more infections than methicillin resistant Staphylococcus aureus (MRSA). These infections are associated with substantial morbidity and mortality including longer hospital stays, neuro-developmental sequelae, and growth impairment. There is limited literature on initiatives to prevent MSSA infections in the NICU. Our NICU saw an increased number of MSSA infections, mainly skin and soft tissue infections (SSTIs), prompting the initiation of this quality improvement (QI) project.
Objective: Our SMART aim was to decrease the total MSSA infections/1000 patient days (PD) from 1.8/1000 PD in our level IV NICU by 20% by June 2024.
Design/Methods: Our QI team performed interventions over 18 months. Baseline data was retrospectively collected from December 2021 to October 2022. Interventions included implementation of MSSA surveillance and decolonization protocols, whole genome sequencing of MSSA isolates to aid with patient cohorting, bare below the elbows (BBE) practice, and enhanced environmental cleaning processes (Figure 1). Our outcome measure included the rate of total MSSA infections. Process measures included the rate of MSSA colonization and adherence to MSSA decolonization, BBE, and central line bundle protocols. Balancing measures included the number of late onset sepsis (LOS) evaluations and antibiotic usage rate (AUR). Statistical process control charts (U- and P-charts) and established Associates in Process Improvement rules for special cause variation were used to display and analyze data.
Results: There was a 78% reduction in the rate of total MSSA infections (from 1.8 to 0.4 infections per 1,000 PD) after initiation of our QI project (Figure 2), primarily driven by a reduction in MSSA SSTIs. The MSSA colonization rate remained stable over time at 19% (Figure 3A). Compliance to the MSSA decolonization protocol, BBE initiative, and central line bundle was 97%, 79% and 99%, respectively (Figure 3B-D). The rates of LOS evaluations and AUR did not increase.
Conclusion(s): An ongoing QI initiative aimed at infection prevention strategies led to a significant decrease in MSSA infections in our level IV NICU, specifically SSTIs. Although rates of MSSA infections decreased, overall MSSA colonization rates did not change over this period highlighting the complex dynamic between colonization and infection, and emphasizing that multipronged strategies are necessary to prevent infection in a NICU.
PDSA cycles for reducing MSSA infections in a level IV NICU.
.jpg) Figure 1. Multiple sequential interventions were performed through 8 PDSA cycles
Figure 1. Multiple sequential interventions were performed through 8 PDSA cycles Monthly total MSSA infections
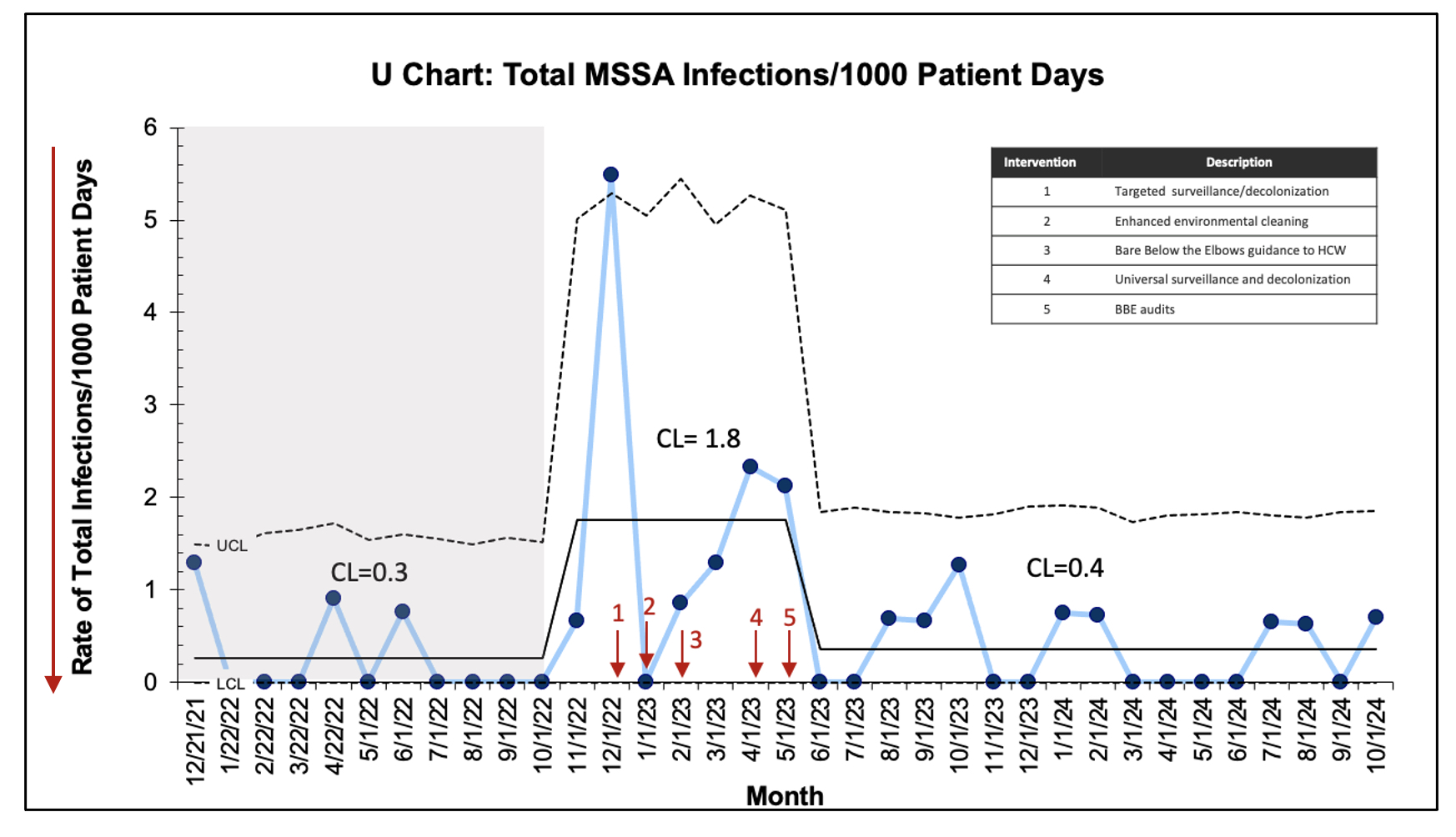 Figure 2. U-chart displaying monthly total MSSA infections per 1000 PD. Arrows indicate interventions. Dashed lines indicate LCL and UCL.
Figure 2. U-chart displaying monthly total MSSA infections per 1000 PD. Arrows indicate interventions. Dashed lines indicate LCL and UCL. SPC charts displaying our process measures: Rate of MSSA colonization and adherence to MSSA decolonization, BBE, and central line bundle protocols.
.jpg) Figure 3. A, P-chart displaying percentage of monthly MSSA colonization in the unit. B, P-chart displaying monthly mupirocin decolonization compliance. C, P-chart displaying monthly compliance with bare below the elbows practice by audits. D, P-Chart displaying monthly central line bundle compliance. Dashed lines indicate LCL and UCL.
Figure 3. A, P-chart displaying percentage of monthly MSSA colonization in the unit. B, P-chart displaying monthly mupirocin decolonization compliance. C, P-chart displaying monthly compliance with bare below the elbows practice by audits. D, P-Chart displaying monthly central line bundle compliance. Dashed lines indicate LCL and UCL. 

