Back
Background: Families with structural determinants of health (SDH) experience decreased communication and less family-centered care. In our NICU, we found that families with SDH were less likely to receive a care conference. Based on their input, we implemented an early care conference entitled a family welcome meeting (FWM) to improve equitable communication. A FWM occurs within one week of NICU admission to provide families of high acuity infants support.
Objective: Determine how often we provided FWM (within and beyond seven days) to qualifying patients. Identify whether significant associations existed between specific SDH and reception of a FWM.
Design/Methods: FWM was a QI initiative beginning July 2021. Data was collected from April 2021 to February 2024 via retrospective chart review. Criteria for receiving a FWM included the following: gestational age less than 30 weeks, surgical diagnosis, hypoxic ischemic encephalopathy, transfer from another NICU, aneuploidy, or primary language other than English (LOE). The four main classes of SDH were race, ethnicity, primary language, and insurance type (as a surrogate for household income). Chi square and logistic regression were used to assess associations between these classes and whether or not a FWM occurred. This analysis was done first for those who received the intervention within seven days and again for those who received the intervention at any time point.
Results: 450 patients qualified for a FWM. 234 (52%) families received the FWM within seven days. An additional 61 families (65%) received one at any time point. While the number of FWM appeared to increase over time (Figure 1a), so too did the number of qualifying families such that the proportion did not exhibit a temporal relationship (Figure 1b). The only SDH that experienced a different rate of FWM was insurance type. Those with private insurance were significantly more likely to receive a FWM as compared to those with public insurance. Results were similar for those who received a FWM within seven days (Figure 2; p= 0.024) and beyond (Figure 3; p= 0.013). There were no interactions between insurance type and other variables.
Conclusion(s): 52% of qualifying families received a FWM within seven days of admission and 65% received a FWM at any time. Patients with public insurance were less likely than those with private insurance to receive a FWM. The goal of improving equitable communication for families with SDH was not met though equality across most categories was achieved. Additional interventions to increase access to FWM for families with lower incomes should be investigated.
Figure 1
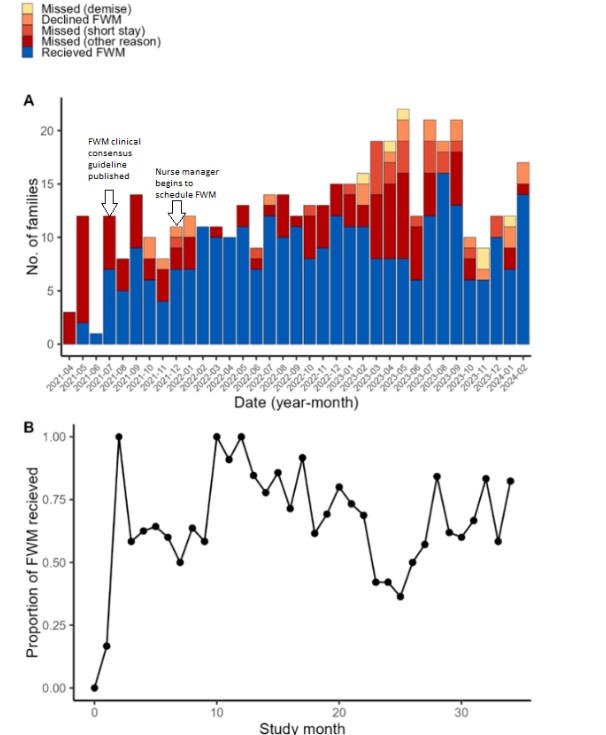 A) The number of families that received a FWM any time (blue) compared to those that did not by study month, due to the demise of the infant (yellow), the family declining the FWM (orange), too short a stay in the NICU (light red), or other reason (dark red). B) The proportion of families that received a FWM at any time out of all those that met the criteria. X-axis displays the number of months starting with first month of the study (2021-04).
A) The number of families that received a FWM any time (blue) compared to those that did not by study month, due to the demise of the infant (yellow), the family declining the FWM (orange), too short a stay in the NICU (light red), or other reason (dark red). B) The proportion of families that received a FWM at any time out of all those that met the criteria. X-axis displays the number of months starting with first month of the study (2021-04).
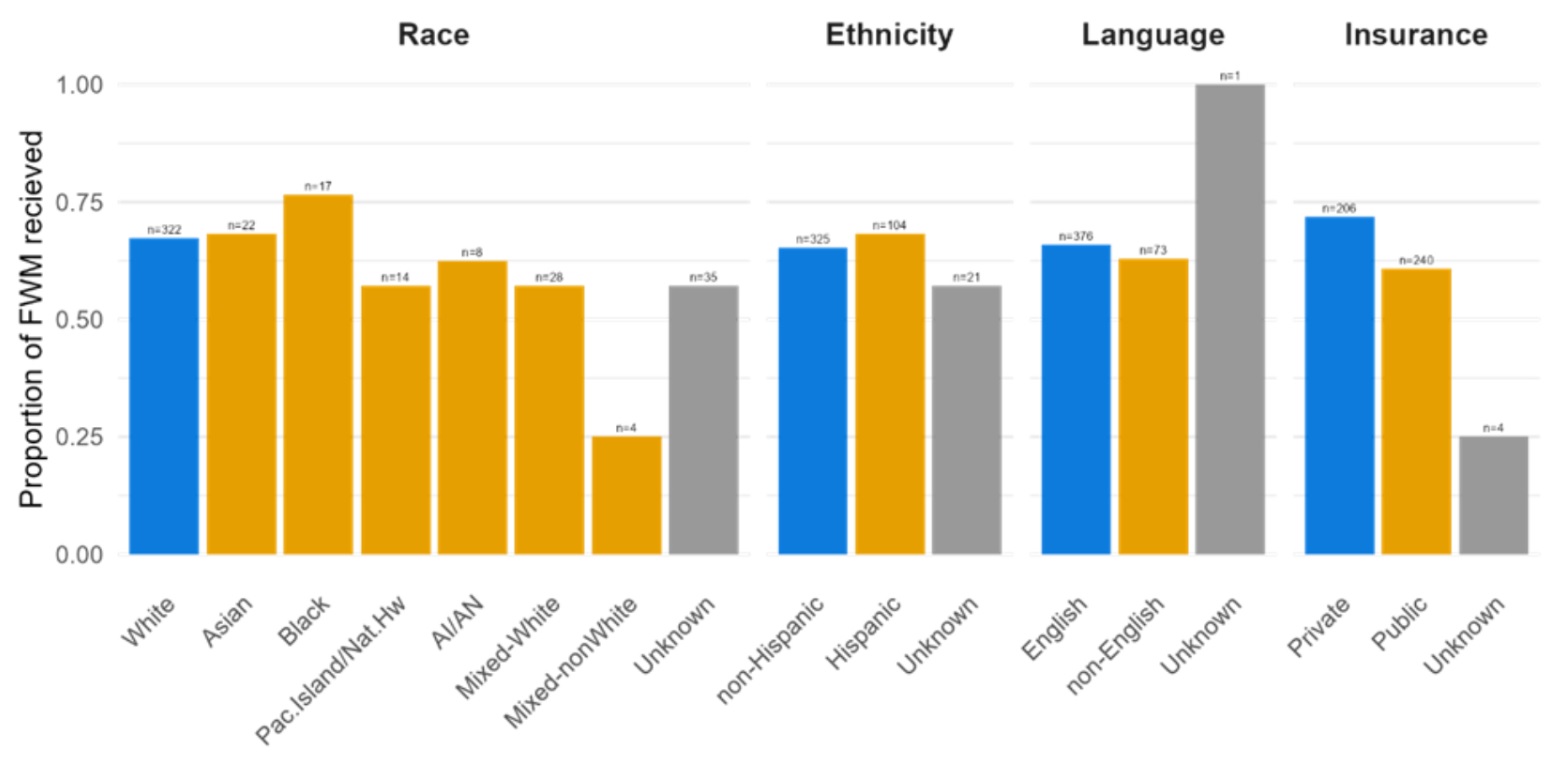
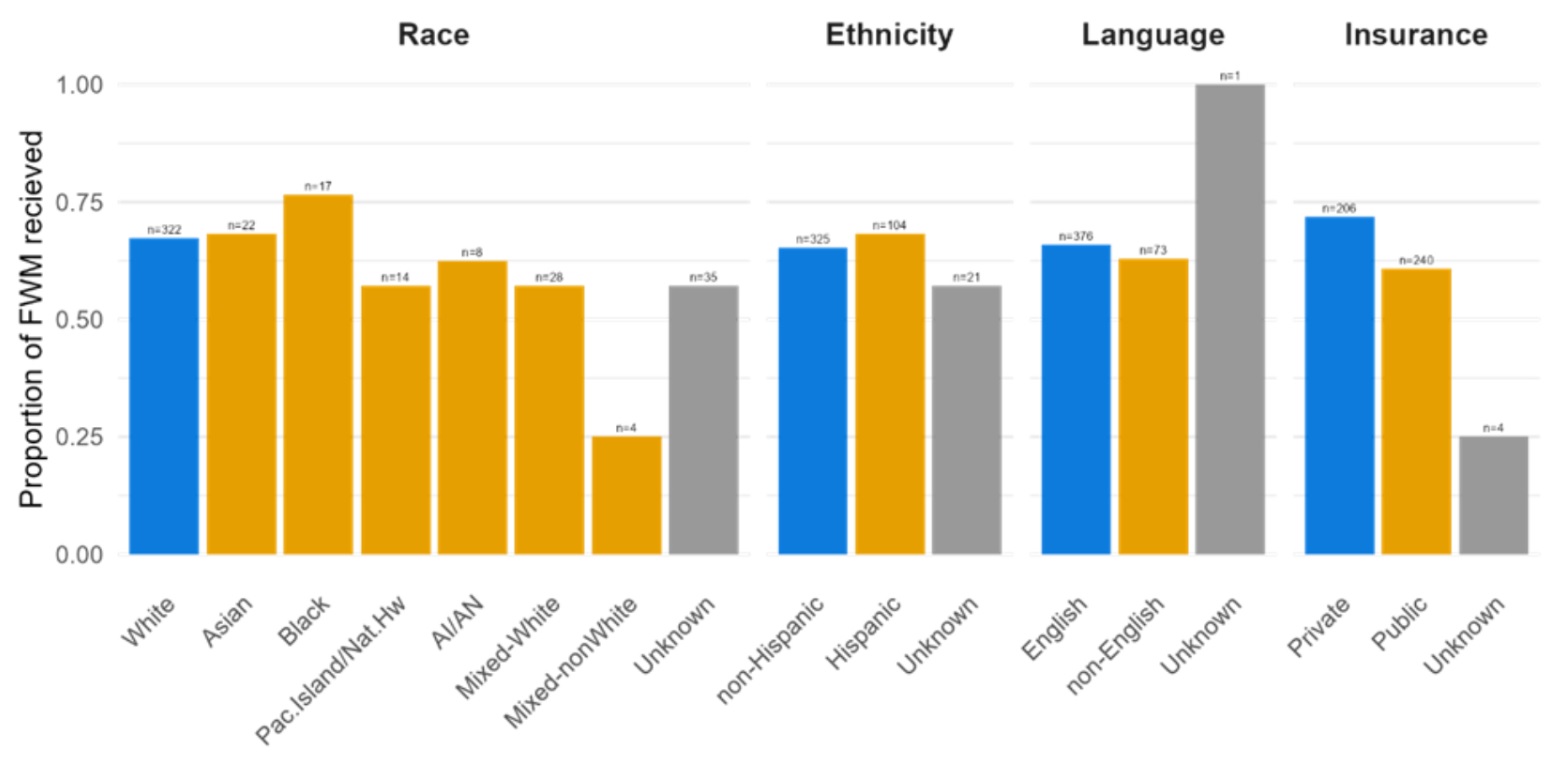
Figure 2
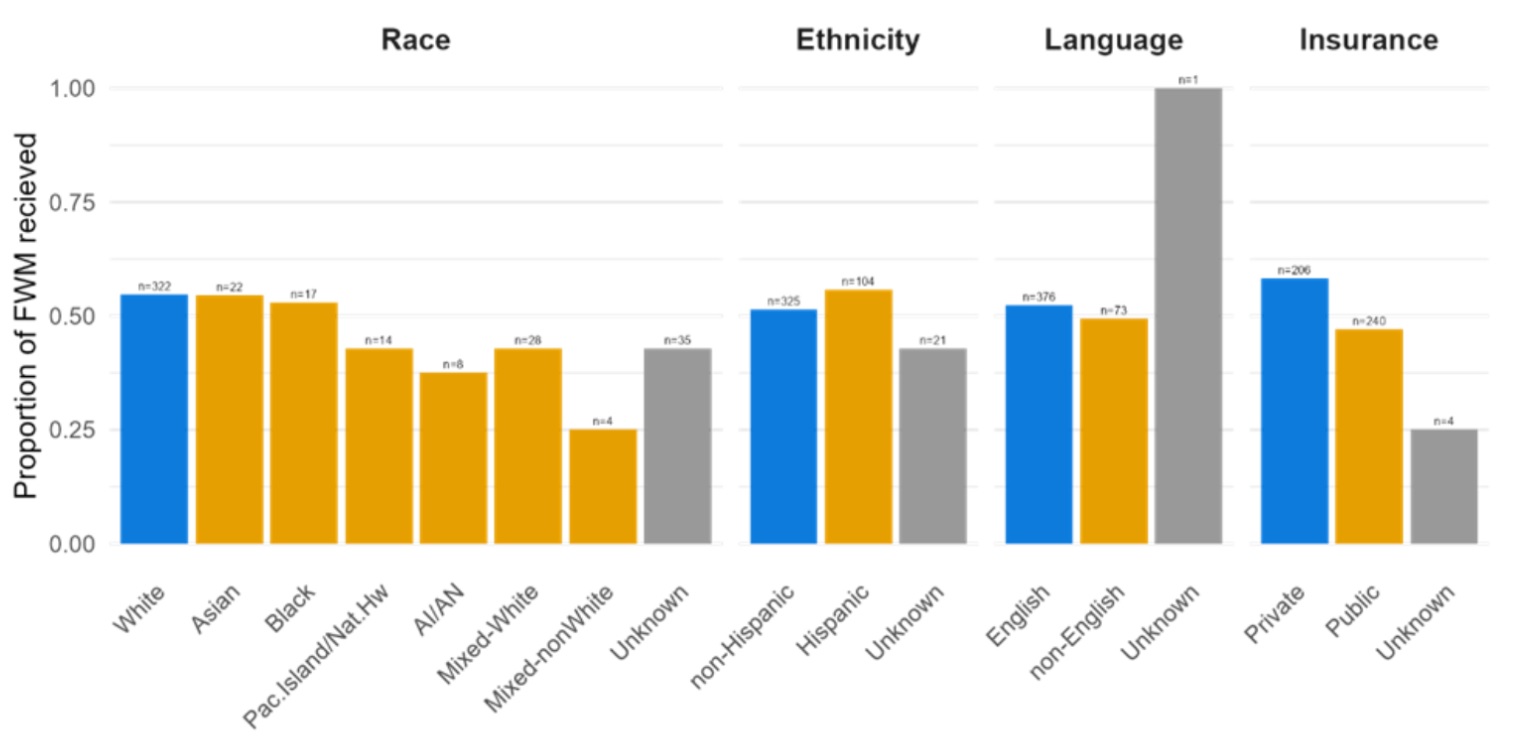 The proportion of qualifying families that received a FWM within seven days of admission over the course of the study separated by race, ethnicity, language and insurance type. SDH categories that may place patients at risk to receive disparate care are displayed in orange, SDH categories at lower risk for disparate care are in blue, and unknown categorization are represented by grey bars. Shown above each bar is the number of families represented by each bar.
The proportion of qualifying families that received a FWM within seven days of admission over the course of the study separated by race, ethnicity, language and insurance type. SDH categories that may place patients at risk to receive disparate care are displayed in orange, SDH categories at lower risk for disparate care are in blue, and unknown categorization are represented by grey bars. Shown above each bar is the number of families represented by each bar.
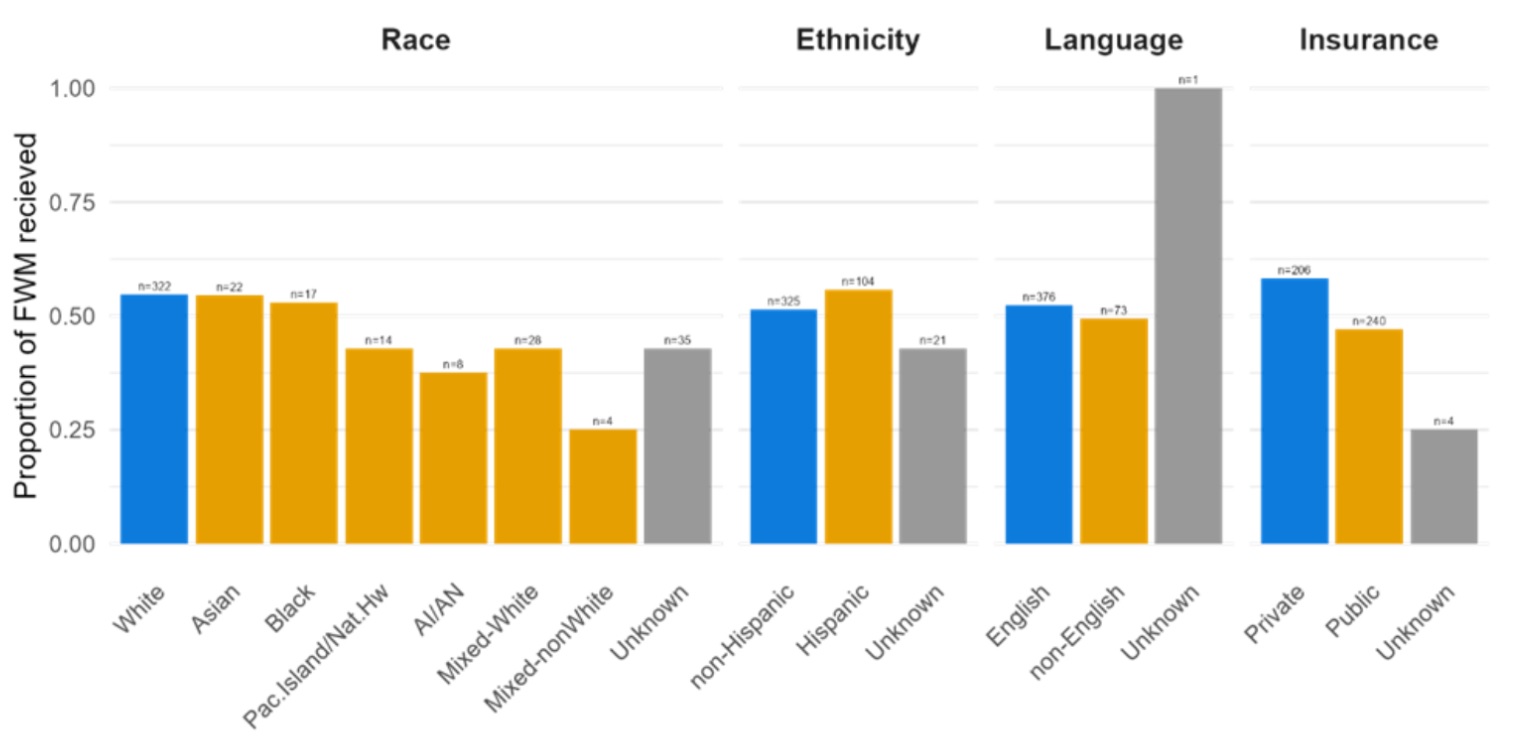
Figure 3
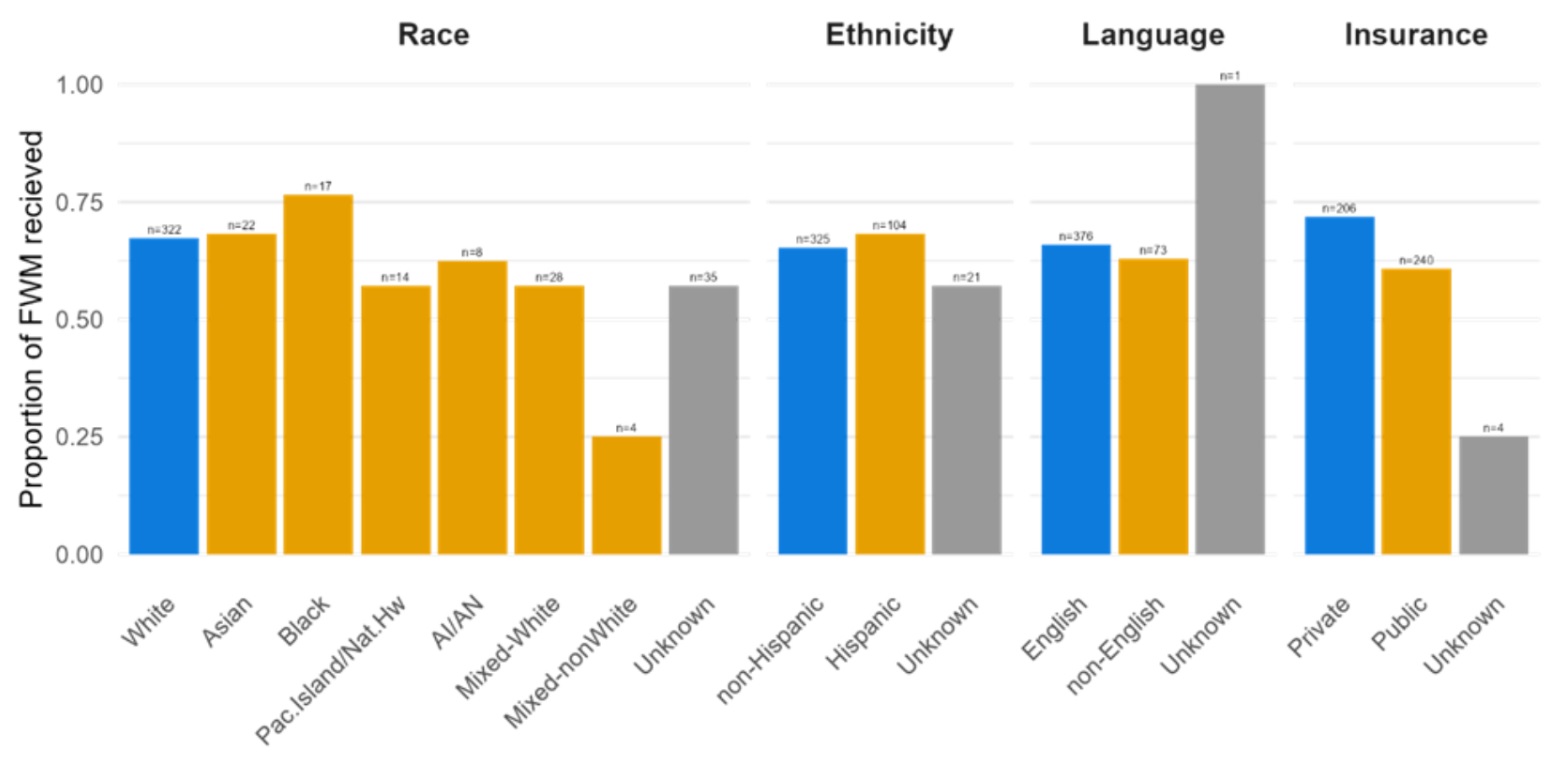 The proportion of qualifying families that received a FWM at any time separated by SDH categories.
The proportion of qualifying families that received a FWM at any time separated by SDH categories.
Figure 1
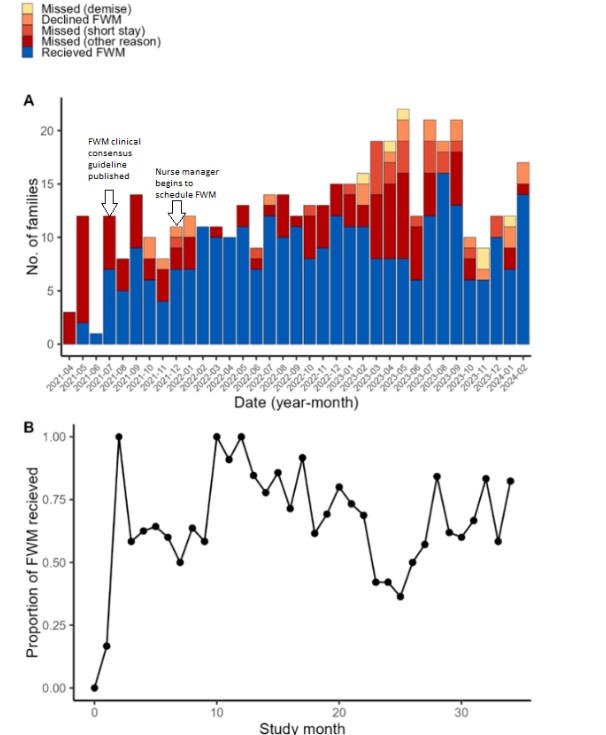 A) The number of families that received a FWM any time (blue) compared to those that did not by study month, due to the demise of the infant (yellow), the family declining the FWM (orange), too short a stay in the NICU (light red), or other reason (dark red). B) The proportion of families that received a FWM at any time out of all those that met the criteria. X-axis displays the number of months starting with first month of the study (2021-04).
A) The number of families that received a FWM any time (blue) compared to those that did not by study month, due to the demise of the infant (yellow), the family declining the FWM (orange), too short a stay in the NICU (light red), or other reason (dark red). B) The proportion of families that received a FWM at any time out of all those that met the criteria. X-axis displays the number of months starting with first month of the study (2021-04).
Figure 2
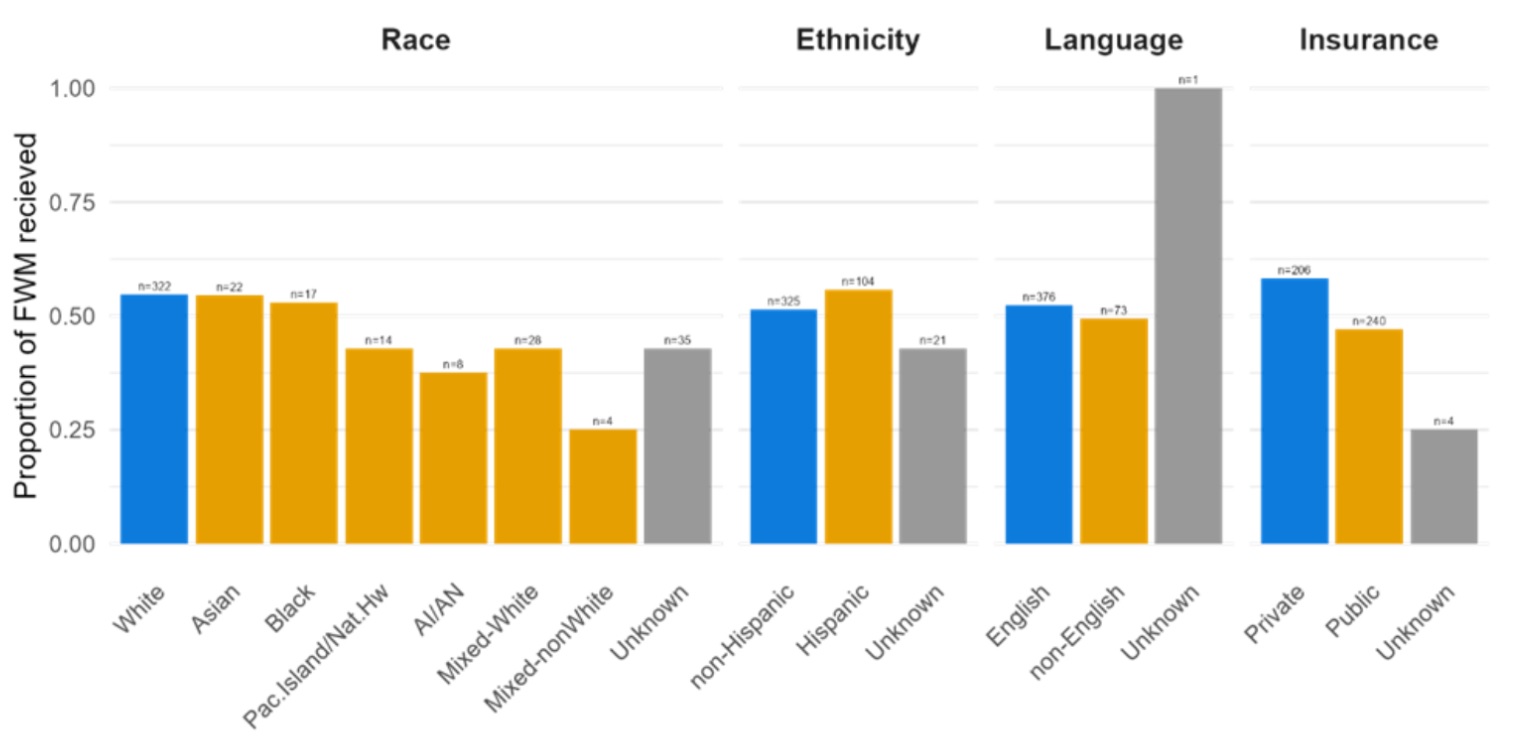 The proportion of qualifying families that received a FWM within seven days of admission over the course of the study separated by race, ethnicity, language and insurance type. SDH categories that may place patients at risk to receive disparate care are displayed in orange, SDH categories at lower risk for disparate care are in blue, and unknown categorization are represented by grey bars. Shown above each bar is the number of families represented by each bar.
The proportion of qualifying families that received a FWM within seven days of admission over the course of the study separated by race, ethnicity, language and insurance type. SDH categories that may place patients at risk to receive disparate care are displayed in orange, SDH categories at lower risk for disparate care are in blue, and unknown categorization are represented by grey bars. Shown above each bar is the number of families represented by each bar.
Figure 3
 The proportion of qualifying families that received a FWM at any time separated by SDH categories.
The proportion of qualifying families that received a FWM at any time separated by SDH categories.
Health Equity/Social Determinants of Health 2
Session: Health Equity/Social Determinants of Health 2
419 - Family Welcome Meetings as a Novel Tool for Early Communication for Families with Structural Determinants of Health in a NICU
Saturday, April 26, 2025
2:30pm – 4:45pm HST
Jane Hwang, Oregon Health & Science University - - Portland, OR, Portland, OR, United States; Jane Y. Hwang, OHSU, Portland, OR, United States; Ladawna Gievers, Doernbecher Children's Hospital at Oregon Health & Science University, Portland, OR, United States; Adam R. Burns, Oregon Health & Science University, Portland, OR, United States; BreAnna Dupuis, Doernbecher Children's Hospital at Oregon Health & Science University, Portland, OR, United States; April D. Castaldi, OHSU, Portland, OR, United States; Shanti Rice, Doernbecher Children's Hospital at Oregon Health & Science University, Portland, OR, United States; Amanda JH. Kim, University of Washington School of Medicine, Seattle, WA, United States
- JH
Jane Hwang, MD
Fellow
Oregon Health & Science University - - Portland, OR
Portland, Oregon, United States
Presenting Author(s)
Background: Families with structural determinants of health (SDH) experience decreased communication and less family-centered care. In our NICU, we found that families with SDH were less likely to receive a care conference. Based on their input, we implemented an early care conference entitled a family welcome meeting (FWM) to improve equitable communication. A FWM occurs within one week of NICU admission to provide families of high acuity infants support.
Objective: Determine how often we provided FWM (within and beyond seven days) to qualifying patients. Identify whether significant associations existed between specific SDH and reception of a FWM.
Design/Methods: FWM was a QI initiative beginning July 2021. Data was collected from April 2021 to February 2024 via retrospective chart review. Criteria for receiving a FWM included the following: gestational age less than 30 weeks, surgical diagnosis, hypoxic ischemic encephalopathy, transfer from another NICU, aneuploidy, or primary language other than English (LOE). The four main classes of SDH were race, ethnicity, primary language, and insurance type (as a surrogate for household income). Chi square and logistic regression were used to assess associations between these classes and whether or not a FWM occurred. This analysis was done first for those who received the intervention within seven days and again for those who received the intervention at any time point.
Results: 450 patients qualified for a FWM. 234 (52%) families received the FWM within seven days. An additional 61 families (65%) received one at any time point. While the number of FWM appeared to increase over time (Figure 1a), so too did the number of qualifying families such that the proportion did not exhibit a temporal relationship (Figure 1b). The only SDH that experienced a different rate of FWM was insurance type. Those with private insurance were significantly more likely to receive a FWM as compared to those with public insurance. Results were similar for those who received a FWM within seven days (Figure 2; p= 0.024) and beyond (Figure 3; p= 0.013). There were no interactions between insurance type and other variables.
Conclusion(s): 52% of qualifying families received a FWM within seven days of admission and 65% received a FWM at any time. Patients with public insurance were less likely than those with private insurance to receive a FWM. The goal of improving equitable communication for families with SDH was not met though equality across most categories was achieved. Additional interventions to increase access to FWM for families with lower incomes should be investigated.
Figure 1
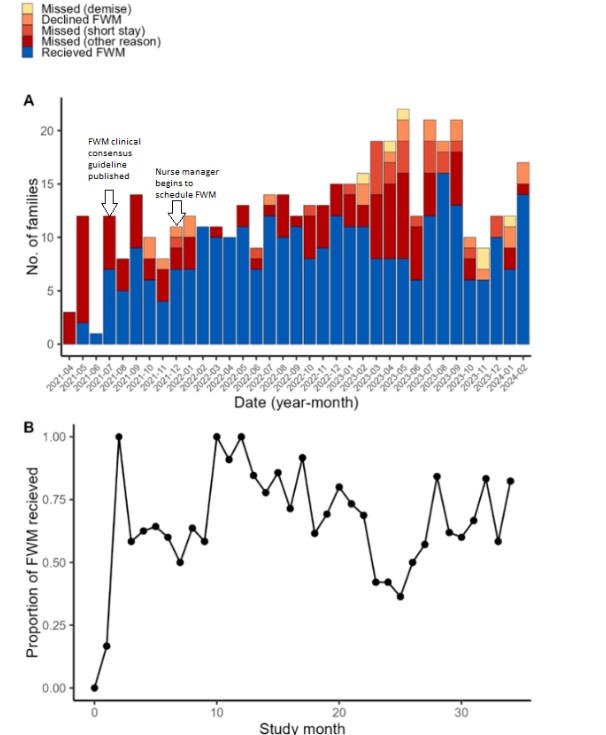 A) The number of families that received a FWM any time (blue) compared to those that did not by study month, due to the demise of the infant (yellow), the family declining the FWM (orange), too short a stay in the NICU (light red), or other reason (dark red). B) The proportion of families that received a FWM at any time out of all those that met the criteria. X-axis displays the number of months starting with first month of the study (2021-04).
A) The number of families that received a FWM any time (blue) compared to those that did not by study month, due to the demise of the infant (yellow), the family declining the FWM (orange), too short a stay in the NICU (light red), or other reason (dark red). B) The proportion of families that received a FWM at any time out of all those that met the criteria. X-axis displays the number of months starting with first month of the study (2021-04). Figure 2
 The proportion of qualifying families that received a FWM within seven days of admission over the course of the study separated by race, ethnicity, language and insurance type. SDH categories that may place patients at risk to receive disparate care are displayed in orange, SDH categories at lower risk for disparate care are in blue, and unknown categorization are represented by grey bars. Shown above each bar is the number of families represented by each bar.
The proportion of qualifying families that received a FWM within seven days of admission over the course of the study separated by race, ethnicity, language and insurance type. SDH categories that may place patients at risk to receive disparate care are displayed in orange, SDH categories at lower risk for disparate care are in blue, and unknown categorization are represented by grey bars. Shown above each bar is the number of families represented by each bar. Figure 3
 The proportion of qualifying families that received a FWM at any time separated by SDH categories.
The proportion of qualifying families that received a FWM at any time separated by SDH categories.Figure 1
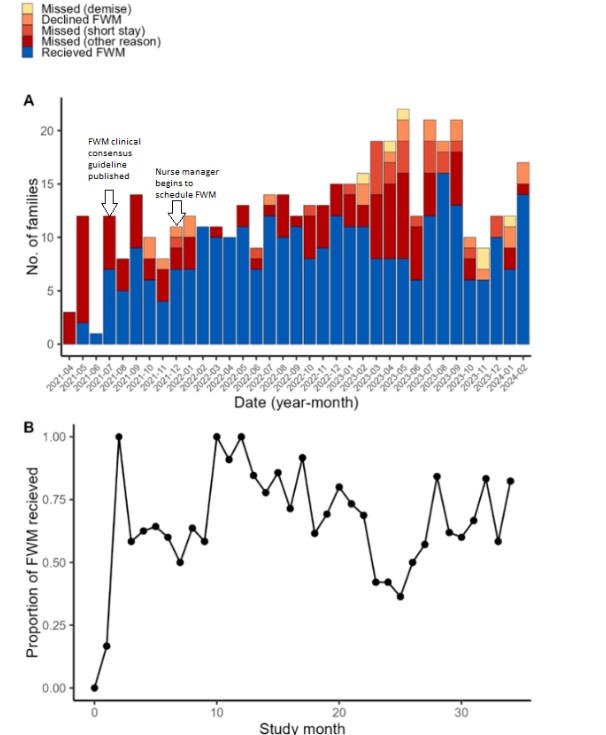 A) The number of families that received a FWM any time (blue) compared to those that did not by study month, due to the demise of the infant (yellow), the family declining the FWM (orange), too short a stay in the NICU (light red), or other reason (dark red). B) The proportion of families that received a FWM at any time out of all those that met the criteria. X-axis displays the number of months starting with first month of the study (2021-04).
A) The number of families that received a FWM any time (blue) compared to those that did not by study month, due to the demise of the infant (yellow), the family declining the FWM (orange), too short a stay in the NICU (light red), or other reason (dark red). B) The proportion of families that received a FWM at any time out of all those that met the criteria. X-axis displays the number of months starting with first month of the study (2021-04). Figure 2
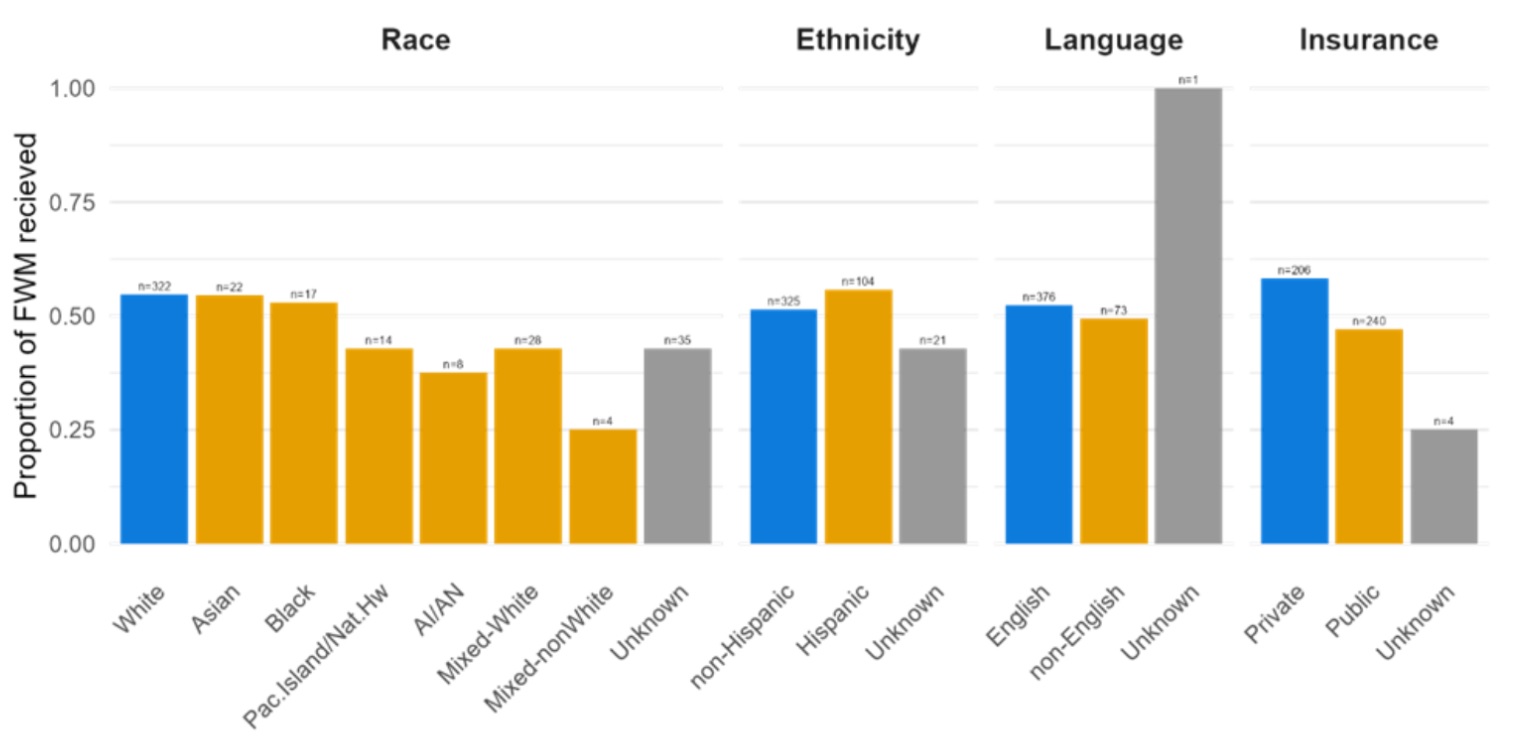 The proportion of qualifying families that received a FWM within seven days of admission over the course of the study separated by race, ethnicity, language and insurance type. SDH categories that may place patients at risk to receive disparate care are displayed in orange, SDH categories at lower risk for disparate care are in blue, and unknown categorization are represented by grey bars. Shown above each bar is the number of families represented by each bar.
The proportion of qualifying families that received a FWM within seven days of admission over the course of the study separated by race, ethnicity, language and insurance type. SDH categories that may place patients at risk to receive disparate care are displayed in orange, SDH categories at lower risk for disparate care are in blue, and unknown categorization are represented by grey bars. Shown above each bar is the number of families represented by each bar. Figure 3
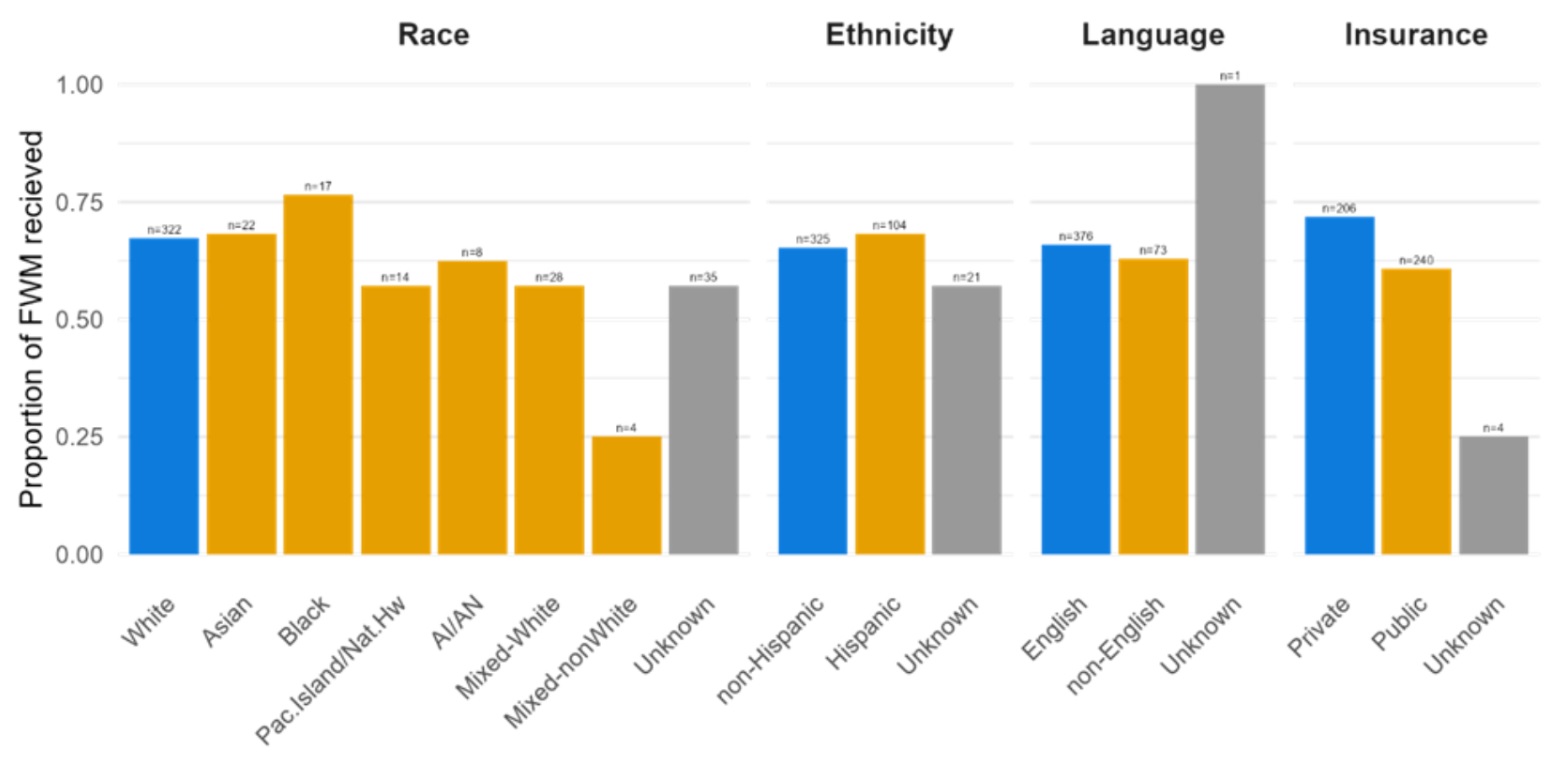 The proportion of qualifying families that received a FWM at any time separated by SDH categories.
The proportion of qualifying families that received a FWM at any time separated by SDH categories.
