Health Equity/Social Determinants of Health 2
Session: Health Equity/Social Determinants of Health 2
413 - Bridging Health Disparities in Neonatal Care: A Systematic Review of Interventions and Screening Tools in the Neonatal Unit
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 413.4545
Behrouz Nezafat Maldonado, Imperial College London, London, England, United Kingdom; Katie Evans, Evelina London Children's Hospital, London, England, United Kingdom

Behrouz Nezafat Maldonado, MBChB MRCPCH (he/him/his)
Resident Doctor
Imperial College London
London, England, United Kingdom
Presenting Author(s)
Background: Social determinants of health (SDOH), shape the conditions of daily living influencing on health and well-being and lead to health disparities. This is particularly relevant for babies admitted to the neonatal intensive care unit (NICU) and their families. Families of preterm infants are disproportionally low-income, and babies with congenital conditions have higher unmet needs. Previous work has highlighted that not many NICU address health disparities. Interventions to reduce SDOH in the NICU are key. Interventions may aim to identify SDOH and enable early help or address SDOH directly. Which specific screening tools or supportive interventions work in the NICU is unknown.
Objective: To systematically review existing screening tools and interventions used in NICU, examine their remit and evaluate their effectiveness.
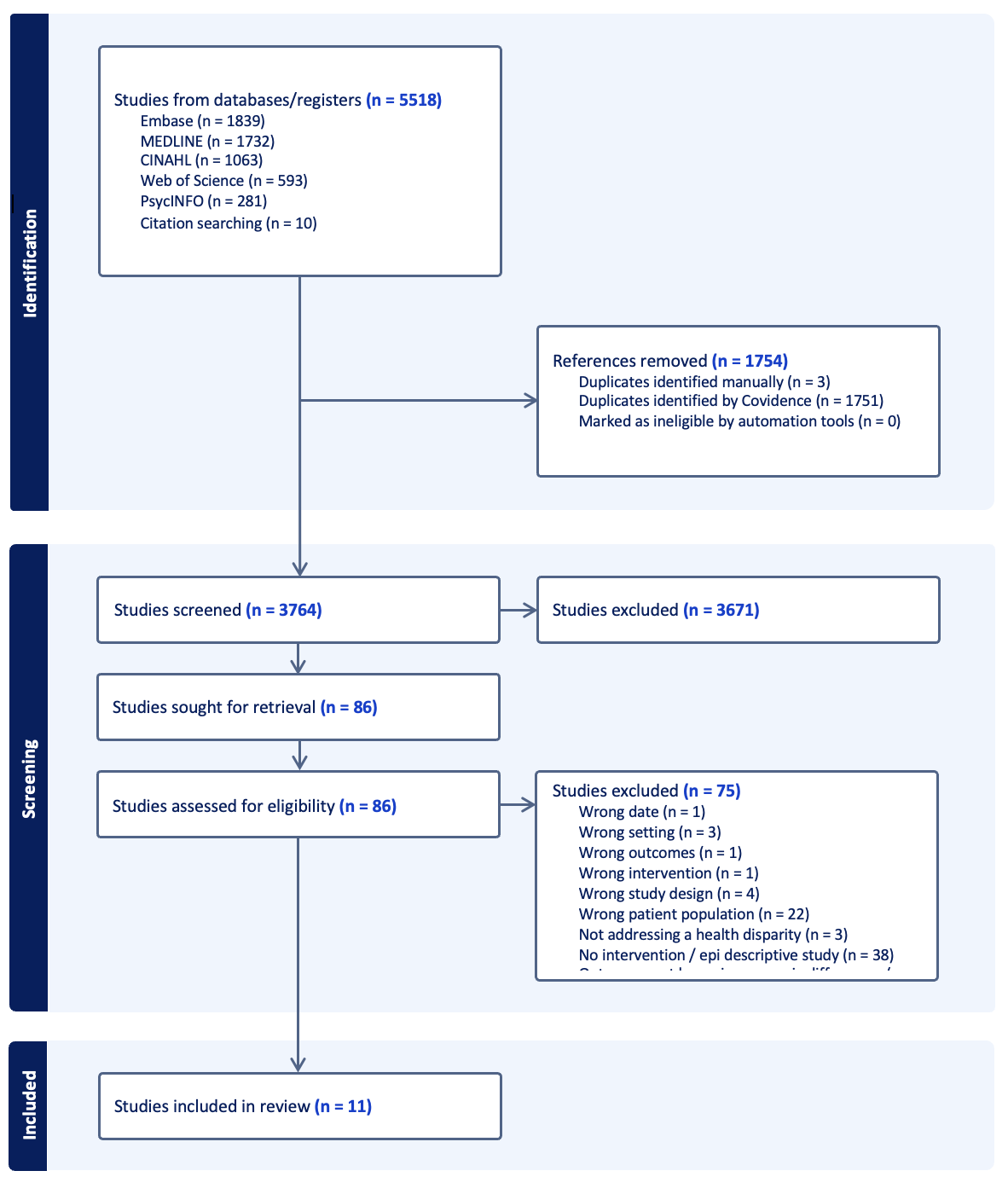
Design/Methods: Systematic review of databases including MEDLINE, Embase, CINAHL, Web of Science and PsychINFO (PROSPERO CRD42024563794). We included interventions that aim to address or identify SDOH in the NICU or postnatal period in any country. We extracted data on the characteristics of the intervention, the SDOH of interest and their effectiveness.
Results: Of 5518 articles identified, 10 studies met the inclusion criteria including 6 screening tools and 4 interventions. A majority of studies were carried out in the US followed by Canada. Screening tools most commonly focused on housing security or parental education. Positive responses in the screening tool led to referrals to social care. All studies reported an increase in detection of at risk families.
2/4 intereventions included were interventions were carried out in NICU in the US, a virtual family care round to increase attendance of parents and a medico-legal partnership to improve assistance to family with unmet social needs. The other two interventions focused on maternal education to improve access to healthcare. A text-message program in Vietnam found that regular messages increased use of healthcare resources and strengthened relationships with health providers. A randomised controlled trial in Ecuador demonstrated that a baby box could be used to improve the likelihood of safer sleep practices amongst low-income families.
Conclusion(s): Several interventions currently exist to identify and reduce SDOH in the postnatal period. Regarding screening, NICU teams should design bespoke tools to fit their population. We found that interventions that improve maternal education on healthcare, postnatal care and public services available and those that improved accessibility to the unit were effective at reducing health disparities.
PRISMA Flow chart