Neonatal Hemodynamics and Cardiovascular Medicine 3
Session: Neonatal Hemodynamics and Cardiovascular Medicine 3
067 - Feasibility of 4D-Echocardiography for RV performance and dimensions in the immediate postnatal neonatal period – a prospective study.
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 67.4635
Sariya Sahussarungsi, McGill University Faculty of Medicine and Health Sciences, Montreal, PQ, Canada; Punnanee Wutthigate, Mahidol university, Bangkok, Krung Thep, Thailand; Jessica Simoneau, Children's Hospital, Vercheres, PQ, Canada; Amanda Ohayon, McGill University Faculty of Medicine and Health Sciences, Montreal, PQ, Canada; Daniela Villegas Martinez, McGill University Faculty of Medicine and Health Sciences, Montreal, PQ, Canada; Catherine Henin, McGill University Faculty of Medicine and Health Sciences, Montreal, PQ, Canada; Tiscar Cavalle-Garrido, McGill University Faculty of Medicine and Health Sciences, Montreal, PQ, Canada; Wadi Mawad, Mcgill university, Montreal, PQ, Canada; Gabriel Altit, McGill University Faculty of Medicine and Health Sciences, Montreal, PQ, Canada; Adrian Dancea, MCH of MUHC, Montreal, PQ, Canada

Sariya Sahussarungsi, MD (she/her/hers)
Fellow
McGill University Faculty of Medicine and Health Sciences
Montreal, Quebec, Canada
Presenting Author(s)
Background: There is limited data on the right ventricular (RV) dimensions and function in newborns using 4D-echocardiography (echo). This imaging technique allows to measure cardiac volumes by capturing all walls of the RV throughout the cardiac cycle. Speckle-tracking echo (STE) allows to reconstruct the cardiac volumes during both contraction and filling phases. Considering the complex RV geometry, this approach may augment the evaluation of common neonatal hemodynamics conditions, such as pulmonary hypertension, congenital heart disease, or right-sided heart failure
Objective: Assess the feasibility of performing 4D-echo in newborns during the immediate postnatal period and to obtain measurements of RV function and dimensions in healthy infants within their first 48 hours of life. The secondary objective was to determine whether factors such as sex, birthweight, body surface area (BSA), body mass index (BMI), or age at echo were associated with the RV end diastolic volume (EDV).
Design/Methods: Prospective observational study recruiting healthy newborns from the nursery at the McGill University Health Centre. Included infants were born following an uncomplicated pregnancy, with no need for resuscitation at birth or admission to the neonatal intensive care unit. RV 4D-echo was done using a Philips X7-2 xMATRIX Transducer with electrocardiogram-gating. A blinded rater, unaware of the subject's details, extracted RV dimensional and functional parameters offline using STE on a TomTec Arena software.
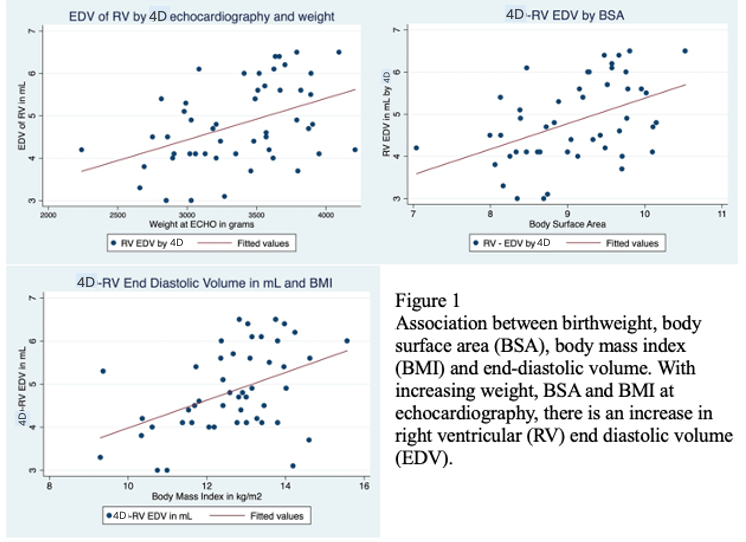
Results: We enrolled 51 newborns, of which 28 (55%) were male. All infants were born at term (mean of 39±1 weeks). Anthropometric measurements were within the expected range for this age group (Table 1). RV 4D-echo was successfully completed in 50 (98%) and was conducted near 24 hours of life. No significant differences were observed between those evaluated before or after 24 hours. By linear regression, RV-EDV was associated to the birthweight (Table 2; p=0.002), BSA (p=0.001), BMI (p=0.002) and end diastolic area obtained by 2D echo in the apical view (p=0.03) - Figure 1, but not to sex or time at echo.
Conclusion(s): We demonstrated the feasibility of assessing RV dimensions and function in neonates using 4D-echo during their transitional period. As expected, RV dimensions were associated with neonatal anthropometric parameters.
Table 1 - Measurement of body metrics
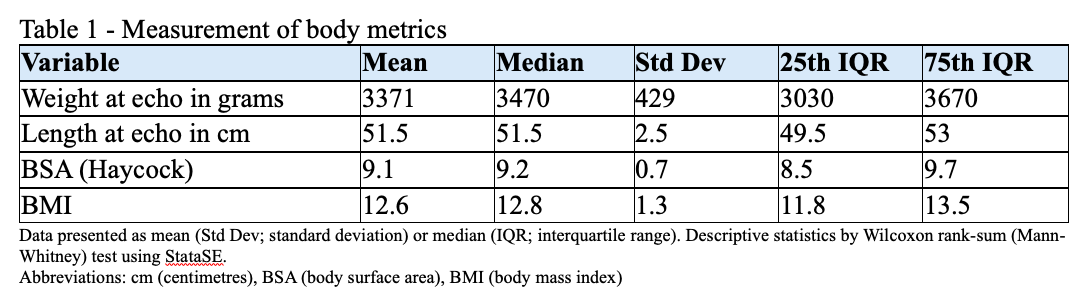
Table 2 - Regression analysis evaluating the association between end diastolic volume and other variables.
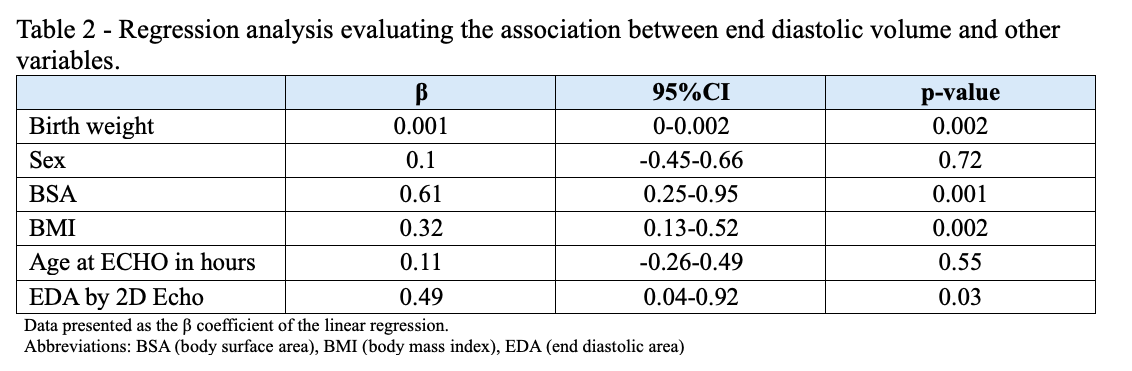
Figure1-Association between birth weight, body surface area(BSA), body mass index(BMI) and end-diastolic volume.
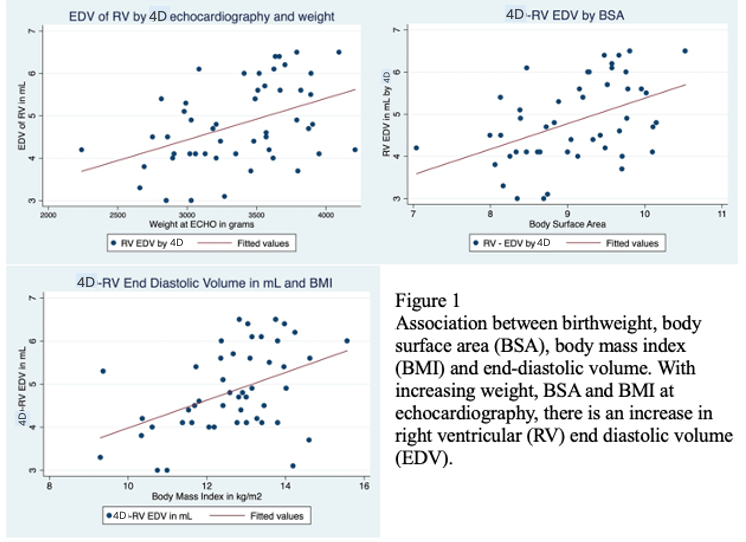
Table 1 - Measurement of body metrics
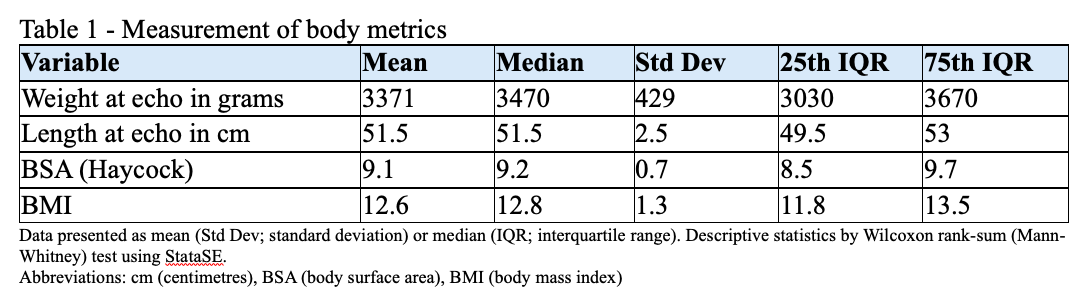
Table 2 - Regression analysis evaluating the association between end diastolic volume and other variables.
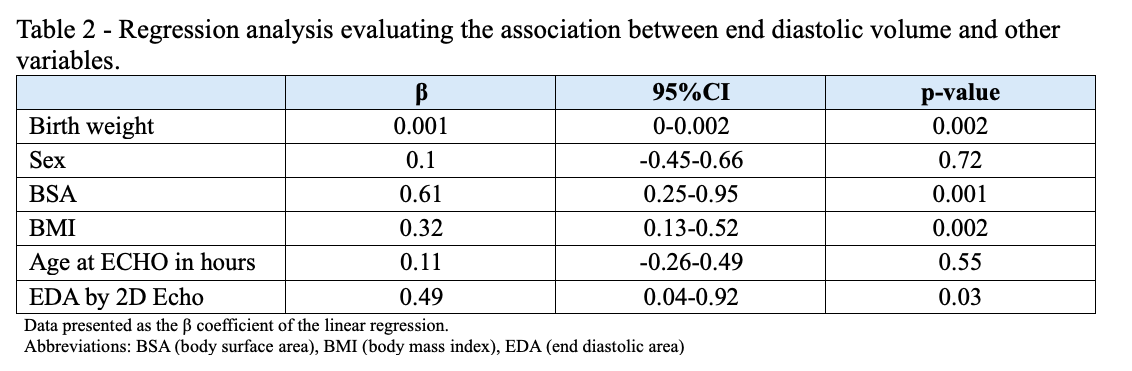
Figure1-Association between birth weight, body surface area(BSA), body mass index(BMI) and end-diastolic volume.