Medical Education 3: Simulation
Session: Medical Education 3: Simulation
206 - Feasibility and Acceptance of Online Simulation to Improve Ventilator Management Knowledge
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 206.4631
Jonathan H. Pelletier, Akron Children’s Hospital, Akron, OH, United States; Danielle Maholtz, Akron Children's Hospital, Akron, OH, United States; Rachel Wojcik, UPMC, Pittsburgh, PA, United States; Craig M. Riley, University of Pennsylvania Health System, West Chester, PA, United States; Roxana R. Amirahmadi, University of Maryland Medical Center, Gaithersburg, MD, United States; Stephanie Maximous, University of Pittsburgh School of Medicine, Pittsburgh, PA, United States; Burton Lee, National Institutes of Health, Bethesda, MD, United States

Jonathan H. Pelletier, MD (he/him/his)
Assistant Professor
Akron Children’s Hospital
Akron, Ohio, United States
Presenting Author(s)
Background: Management of mechanical ventilation is an Accreditation Council for Graduate Medical Education core competency for pediatric and adult critical care medicine, anesthesiology, and emergency medicine. However, there is no standard approach to teaching mechanical ventilation, resulting in poor learning outcomes. Nationally, less than 50% of fellows are satisfied with their ventilator training. Both trainees and attendings score poorly on standardized assessments.
Objective: To develop and evaluate the feasibility and acceptance of a simulation-based online ventilator education tool accompanying a mechanical ventilation course.
Design/Methods: We conducted a prospective, open-label, pilot cohort study of adult or pediatric critical care fellows and attendings enrolled in a year-long multi-institutional virtual mechanical ventilation preceptorial course. The course is organized into eight chapters. Each chapter has associated reading materials, challenge questions, and clinical cases. We developed the Preceptorial Online Ventilator Education tool (PrOVE) and offered it to the learners in the course on a voluntary basis. The primary outcomes were simulator use and learner satisfaction. Secondary outcomes included course completion rates and examination scores compared against a historical control.
Results: PrOVE was successfully developed including reading materials (Figure 1), interactive ventilator waveforms (Figure 2), and patient cases (Figure 3). 64% (43/67) course participants used the online simulator for 184 hours on the first chapter, including 27/42 fellows and 16/23 attendings. 95% (41/43) provided demographic information. 44% (18/41) respondents had taken a prior ventilator course, and participants had a median (IQR) of 22 (12-32) prior hours of formal ventilator training. 80% (33/41) of participants were directly responsible for making ventilator changes in their ICU and 80% (33/41) taught mechanical ventilation either formally or informally. 77% (33/43) provided simulator feedback. 100% (33/33) reported that use of PrOVE improved their learning, and 88% (29/33) stated the stimulator was easy to use. Participants reported a median (IQR) of 3 (2-4) hours of simulator use on the first chapter. 100% (67/67) learners completed the first preceptorial chapter. Further completion and examination scores will be reported in December 2024.
Conclusion(s): PrOVE was voluntarily adopted by 64% of critical care physicians enrolled in a mechanical ventilation preceptorial course, with high rates of user satisfaction. Further data collection is required to determine effects on course dropout rates and final scores.
Figure 1. Sample Reading Materials.
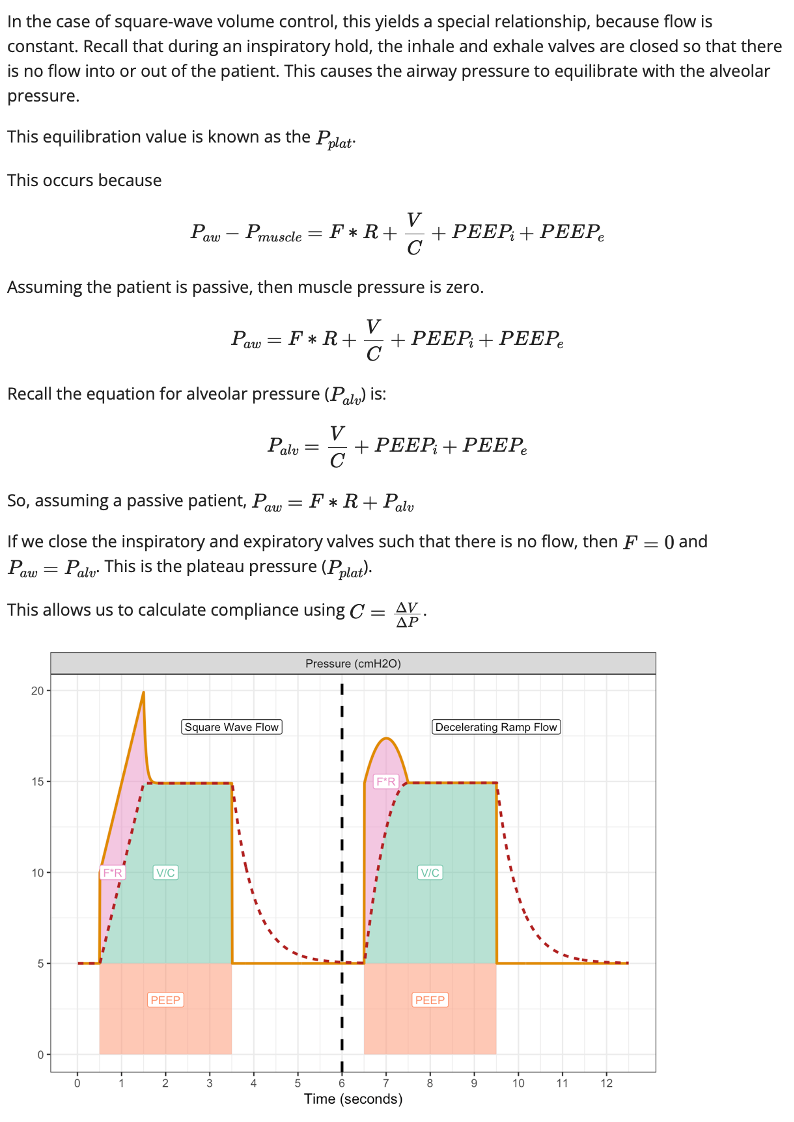 Sample reading materials from the "volume control" chapter of PrOVE.
Sample reading materials from the "volume control" chapter of PrOVE.Figure 2. Sample Interactive Waveforms.
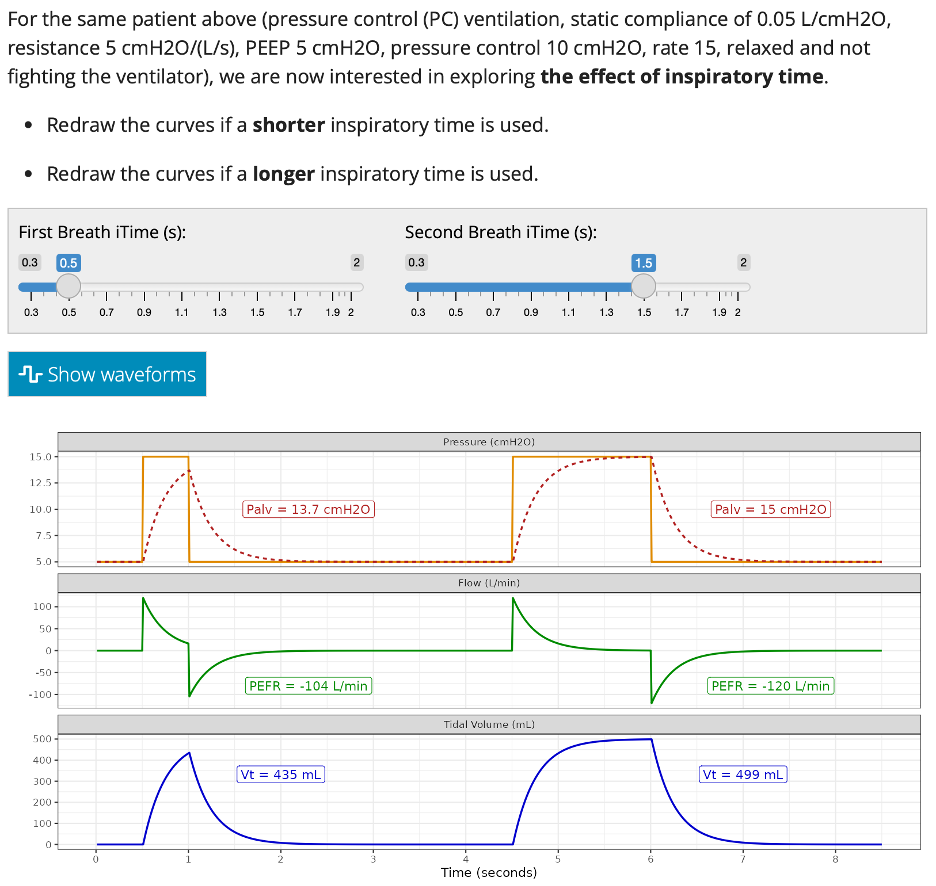 Sample interactive waveforms from the "pressure control" chapter of PrOVE.
Sample interactive waveforms from the "pressure control" chapter of PrOVE.Figure 3. Sample Patient Case.
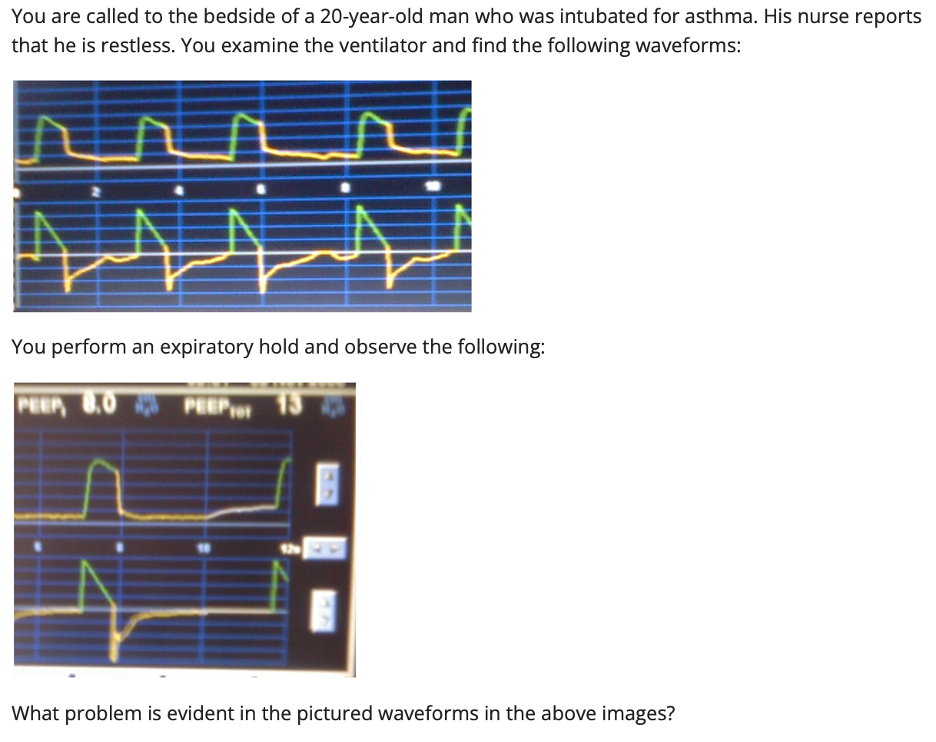 Sample patient case from the "expiratory waveforms" chapter of PrOVE.
Sample patient case from the "expiratory waveforms" chapter of PrOVE.Figure 1. Sample Reading Materials.
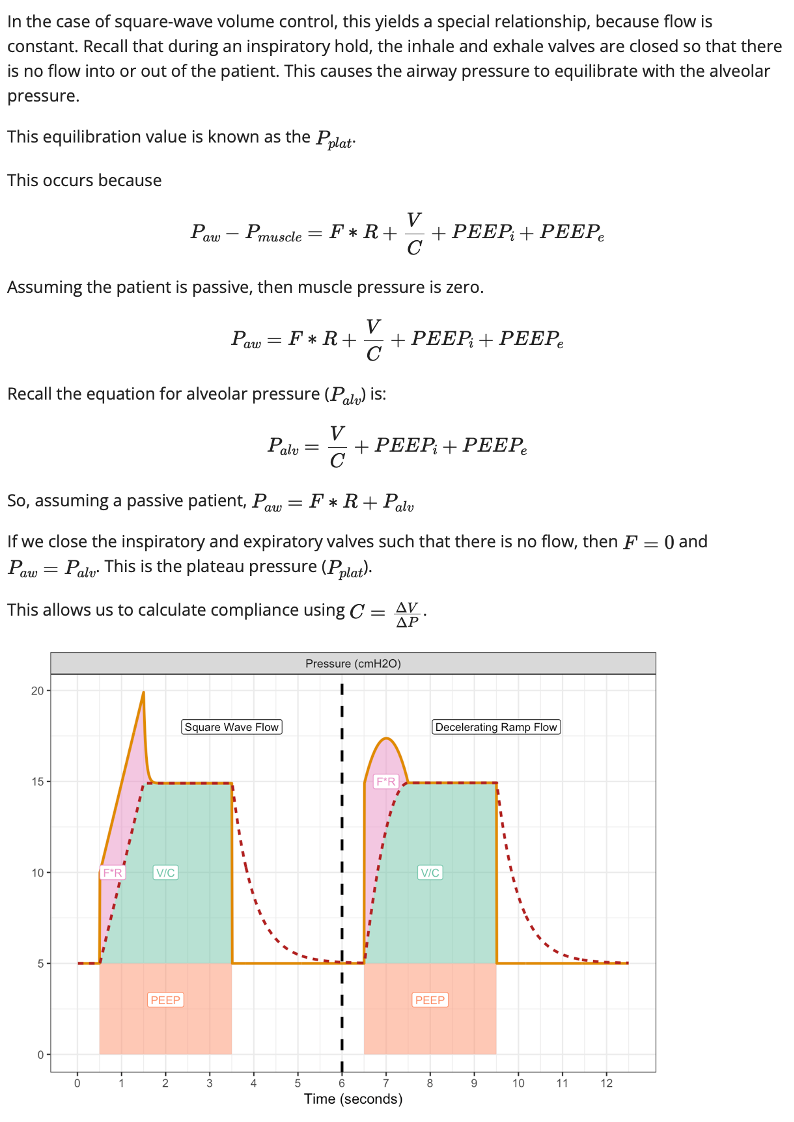 Sample reading materials from the "volume control" chapter of PrOVE.
Sample reading materials from the "volume control" chapter of PrOVE.Figure 2. Sample Interactive Waveforms.
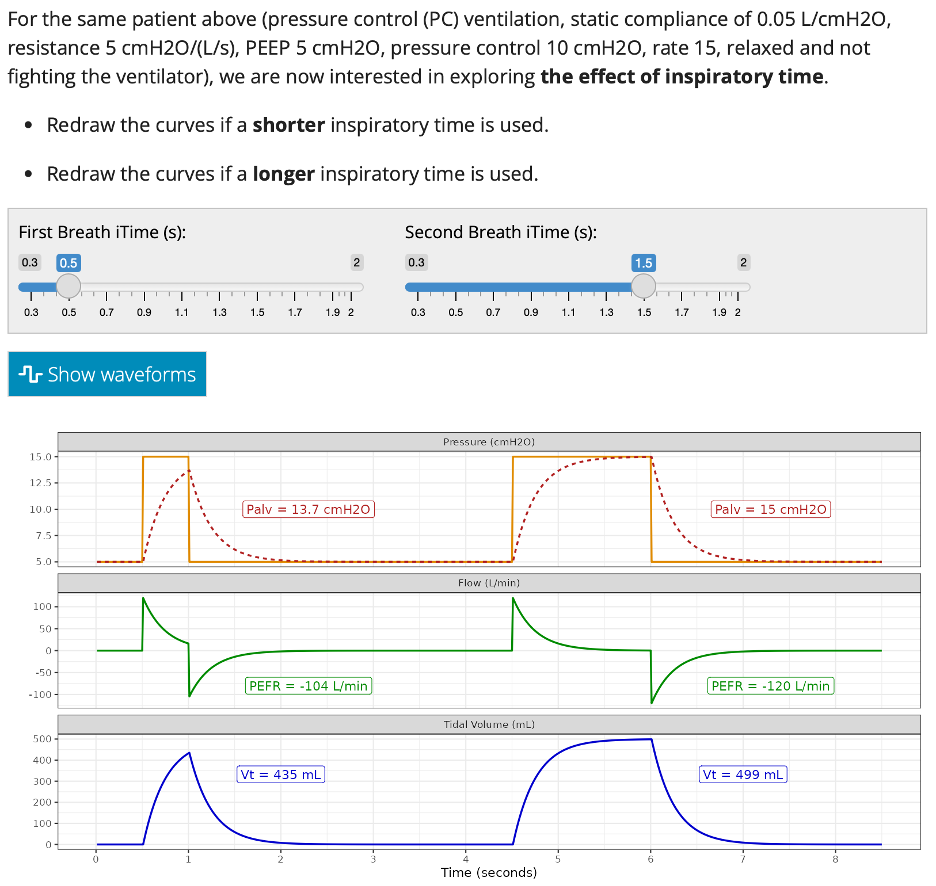 Sample interactive waveforms from the "pressure control" chapter of PrOVE.
Sample interactive waveforms from the "pressure control" chapter of PrOVE.Figure 3. Sample Patient Case.
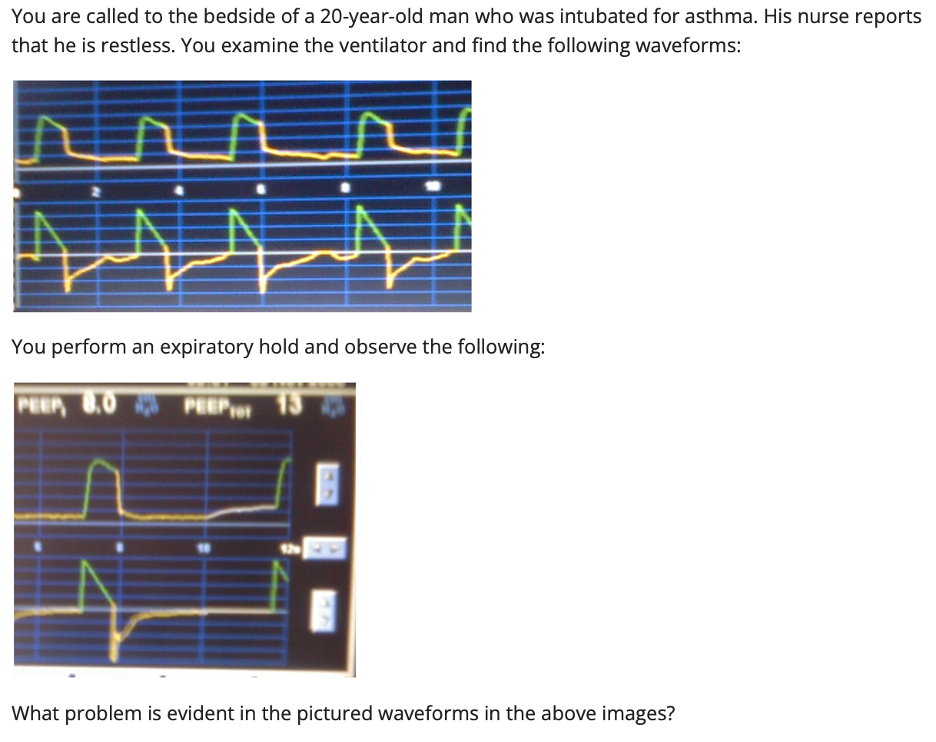 Sample patient case from the "expiratory waveforms" chapter of PrOVE.
Sample patient case from the "expiratory waveforms" chapter of PrOVE.
