Medical Education 5: Procedures and Simulation
Session: Medical Education 5: Procedures and Simulation
229 - Digital versus Traditional Otoscopy: Comparing Diagnostic Accuracy and Trainee Confidence in the Pediatric Ear Exam
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 229.4430
Suzanne Coles, Dell Children's Medical Center of Central Texas, Austin, TX, United States; Jennifer Duc, Dell Children's Medical Center of Central Texas, Austin, TX, United States

Suzanne Coles, MD (she/her/hers)
Resident
Dell Children's Medical Center of Central Texas
Austin, Texas, United States
Presenting Author(s)
Background: The pediatric ear exam is difficult for learners to master without hands-on practice and confirmation of their findings by a more experienced provider. Acute otitis media, the most commonly identified pathology in pediatric ear exams, can lead to complications such as tympanic membrane rupture and conductive hearing loss if underdiagnosed, while overdiagnosis risks unnecessary antibiotic use and associated side effects. Prior surveys have shown low confidence in diagnostic ability with otoscopy and dissatisfaction with otoscopy training among medical trainees.
Objective: This study investigates whether using a digital otoscope to review findings and provide real-time feedback to pediatric residents in a continuity clinic setting can improve diagnostic agreement between residents and attendings, and enhance resident confidence in performing otoscopic exams.
Design/Methods: A digital otoscope was purchased for use in the clinic using a medical education grant. Pediatric residents in a primary care continuity clinic were randomized to use a traditional or digital otoscope for clinically indicated ear exams over a six month period. After the resident diagnosis was recorded, the attending separately examined the patient with the same otoscope, recorded the final diagnosis, and provided feedback. For exams conducted with the digital otoscope, recorded video images were reviewed jointly. A five-point Likert scale survey assessed residents' confidence in otoscopic technique before and after the study period.
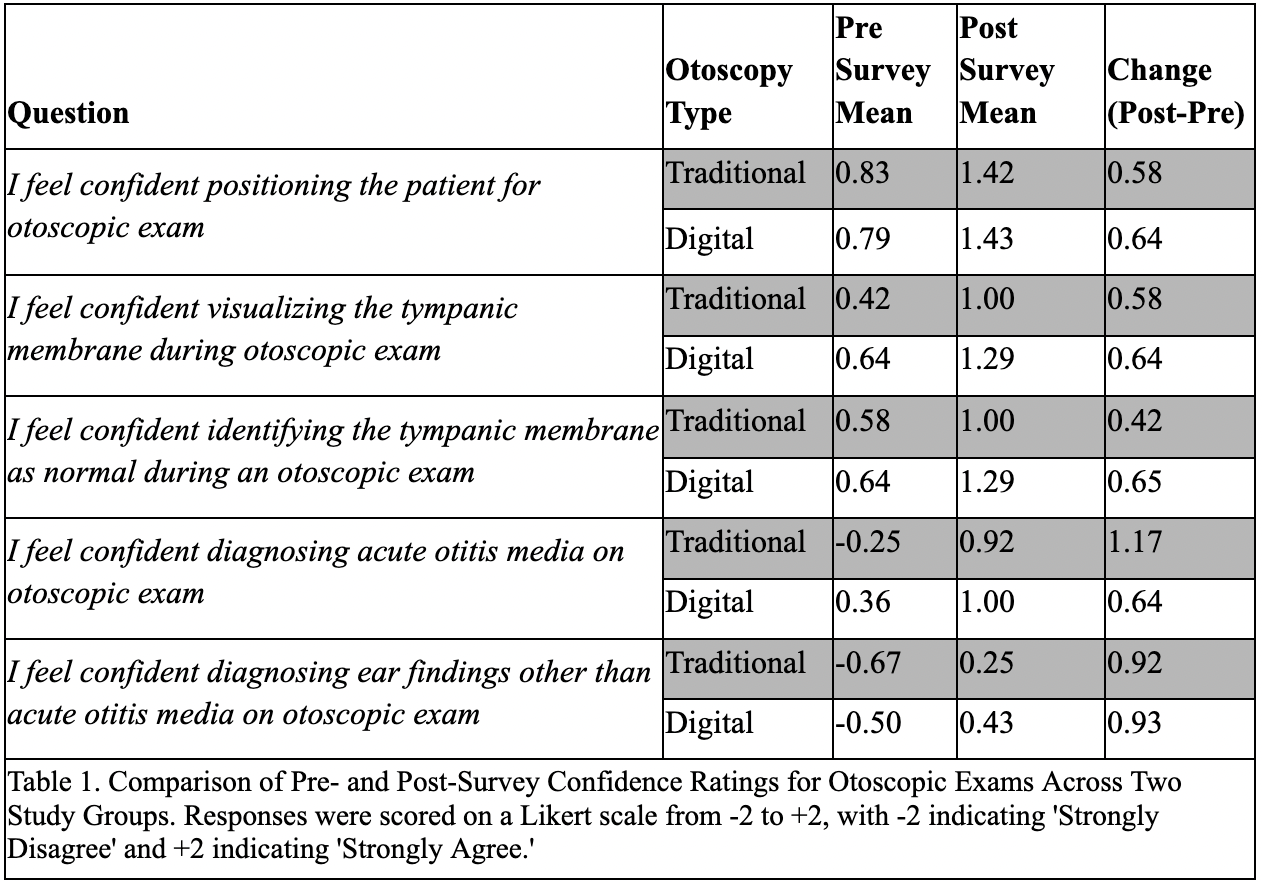
Results: The digital otoscope group showed a higher resident-attending agreement rate (62%, 21/34) compared to the traditional group (54%, 27/50) (p=0.48), particularly in the early months of the study, with a gradual decline over time (Figure 1). Fewer treatment plan changes were needed after attending exams in the digital group (18%, 5/34) compared to the traditional group (26%, 13/50; Figure 2) (p=0.22). Both groups demonstrated increased confidence in otoscopy skills after the study (Table 1).
Conclusion(s): Both groups of residents reported increased confidence in otoscopic skills after six months. Although there was an initial trend toward higher diagnostic agreement and fewer treatment plan changes in the digital otoscopy group, these differences were ultimately not statistically significant. These results suggest that though digital otoscopy offers promising educational benefits through image review and real-time feedback, further research with larger sample sizes are necessary to fully assess its impact on diagnostic accuracy and clinical decision making in pediatric otoscopy training.
Figure 1. Percent agreement over time between resident and attending physical exam findings using digital and traditional otoscopes.
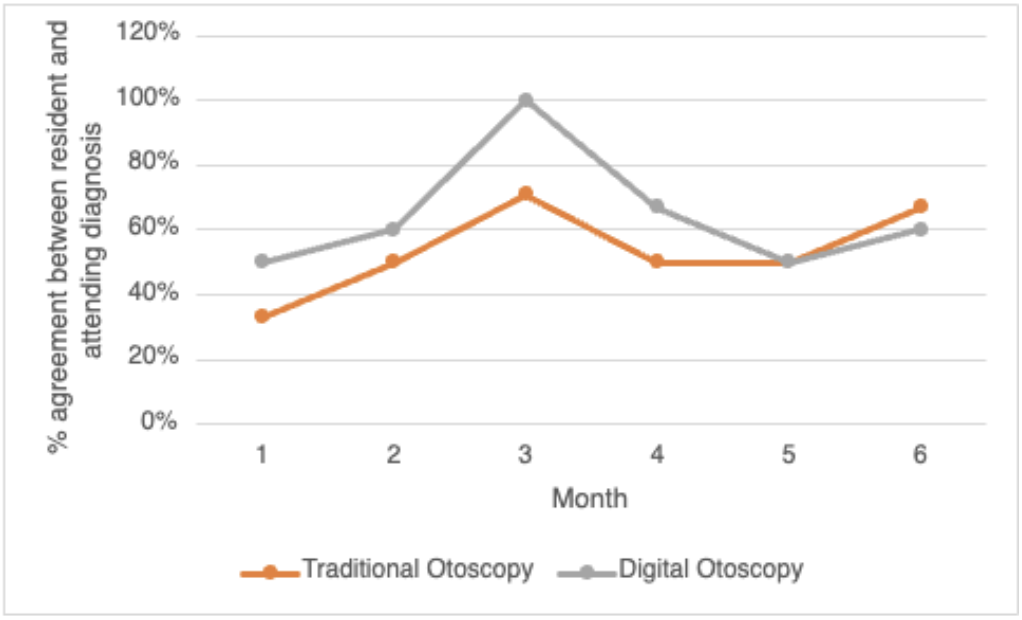
FIgure 2. Number of clinically-significant diagnosis changes between resident and attending exam with traditional otoscopy versus digital otoscopy.
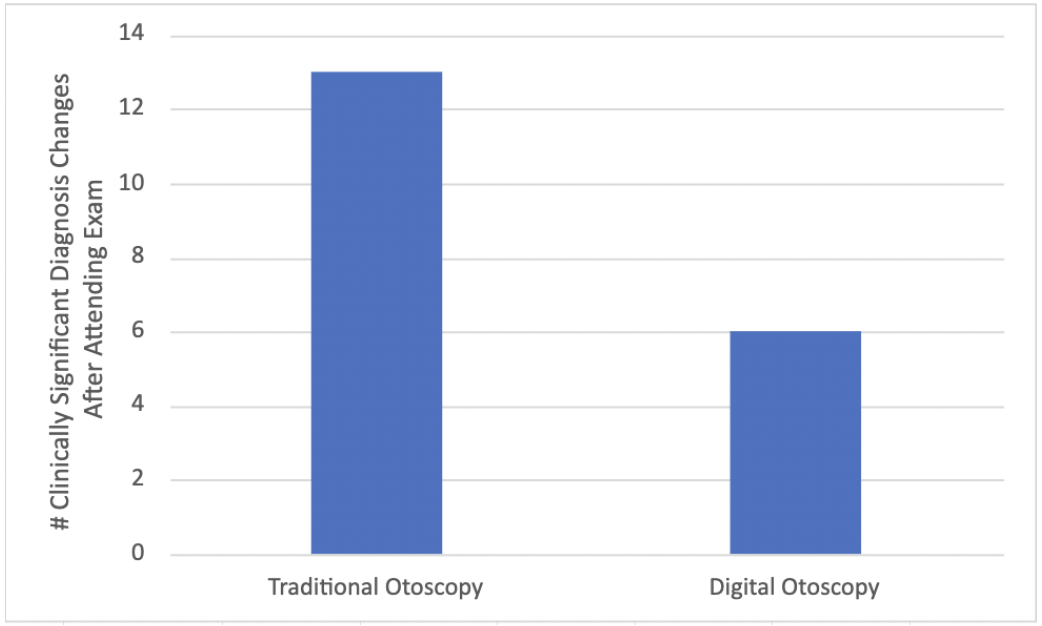
Table 1. Comparison of pre- and post-survey confidence ratings for otoscopic exams across two study groups. Responses were scored on a Likert scale from -2 to +2, with -2 indicating 'Strongly Disagree' and +2 indicating 'Strongly Agree.'