Children with Chronic Conditions 3
Session: Children with Chronic Conditions 3
465 - The Effect of Race and Economic Status on Pediatric Diabetes and Asthma Admissions in the United States
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 465.6899
Madhuradhar Chegondi, University of Illinois College of Medicine, Peoria, IL, United States; Prithvi Sendi, Florida International University Herbert Wertheim College of Medicine, Miami, FL, United States; Balagangadhar R. Totapally, Nicklaus Children’s Hospital, Miami, FL, United States

Madhuradhar Chegondi, MD
Visiting Clinical Professor
University of Illinois College of Medicine
Peoria, Illinois, United States
Presenting Author(s)
Background: Socioeconomic status (SES) is crucial to healthcare accessibility and patient care quality. The SES impacts the prevalence and outcomes of chronic diseases such as diabetes mellitus (DM) and asthma.
Objective: To evaluate the association between SES indicators and hospitalization rates for diabetes and asthma, as measured by the Agency for Healthcare Research and Quality's Pediatric Quality Chronic Composite 92 (PDI 92).
Design/Methods: We analyzed 2016 to 2019 Kids' Inpatient Databases and used a weighted sample to obtain national outcome estimates. We included children aged 6 to 17 years hospitalized with diagnoses of DM and asthma, using ICD-10 codes. We compared the demographics, including race/ethnicity, household income quartiles, patient location, insurance type, hospital length of stay (LOS), charges, and mortality rates between all discharges and discharges with DM or asthma. Statistical analysis was performed using chi-squared test, Mann-Whitney U test, and regression models.
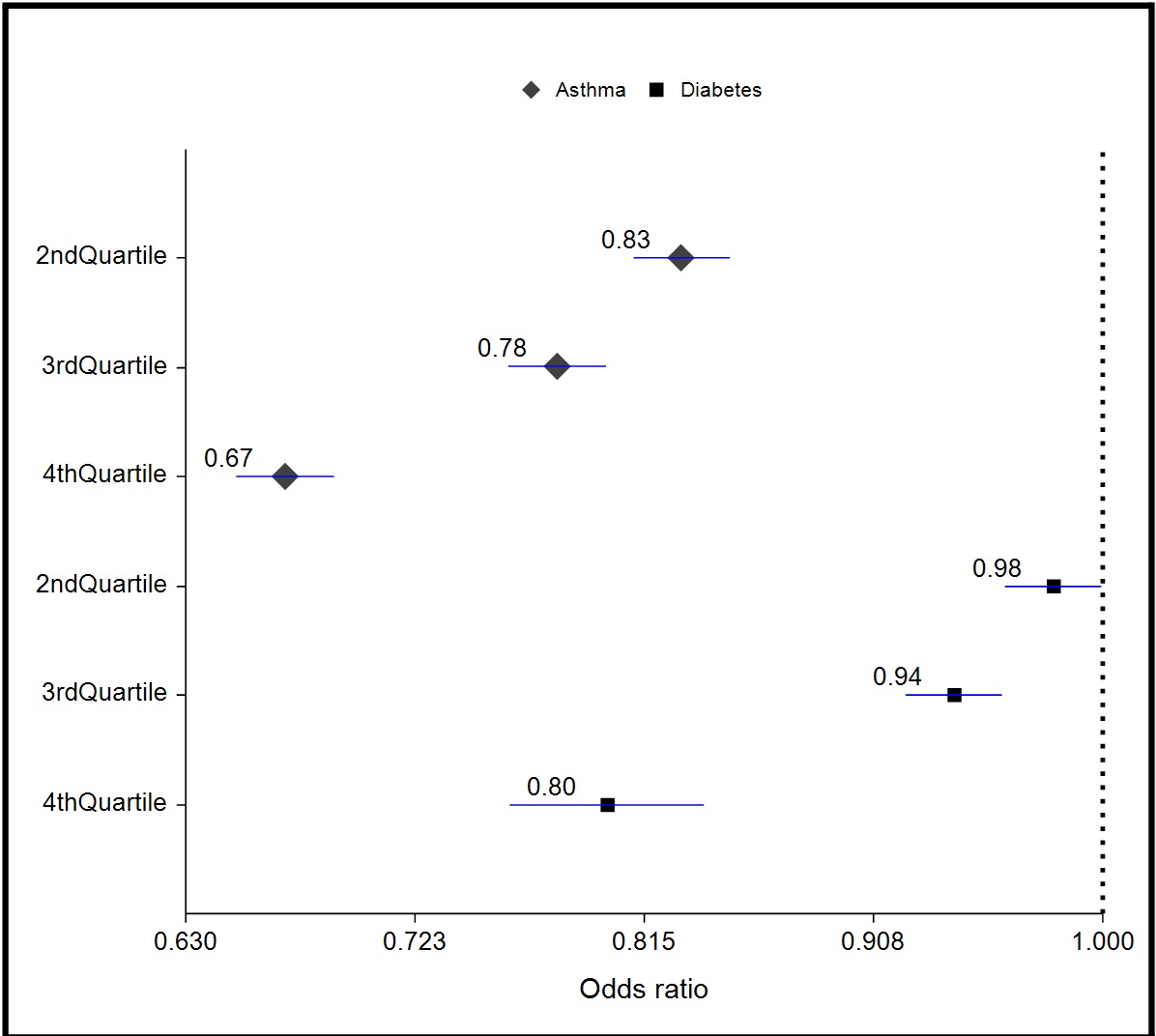
Results: The total number of discharges between 2016 and 2019 was 1.7 million. Out of them, 43,177 (2.5%) had a primary diagnosis of DM, and 70,684 (4%) had asthma. The median age for children with diabetes was 13 years (IQR 11-16), whereas in the asthma group was 9 years (IQR 7-12). Baseline demographics and outcomes are summarized in Table 1. Among the hospitalized patients with DM, mostly were White (49.7%), and in asthma were Black (39.1%). A significant proportion of children with diabetes (33.9%) and asthma (42.3%) were from zip codes with the lowest income quartile (p value < 0.001). Mortality rates during hospitalization among groups are similar and very low, 0.1%. Both groups' binary logistic regression analysis showed a significant association between the outcomes and demographics, including age, race, income, patient location, and payor type (Table 2). Adjusted odds of hospitalization were lower in the higher income quartile compared to 1st quartile (Figure).
Conclusion(s): The proportion of lower-income and racial minority children was higher among hospitalized children with diabetes and asthma. Improved preventive and ambulatory services for at-risk populations could decrease hospitalization of children with these ambulatory care-sensitive conditions.
Table 1. Baseline demographics and outcomes of children with diabetes with complications and asthma
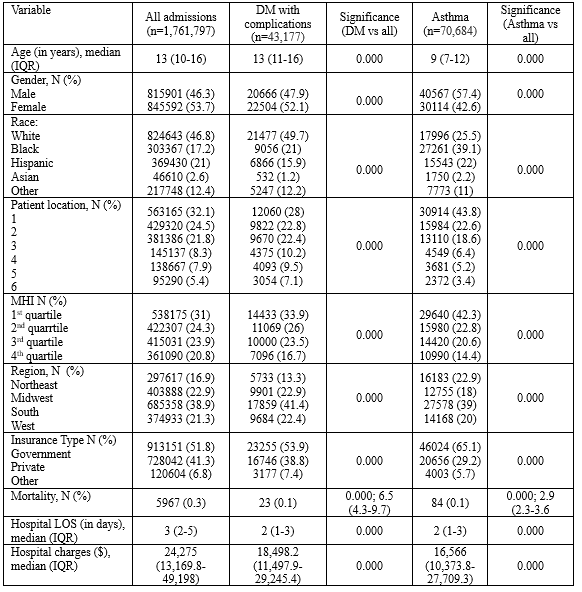 DM = diabetes; IQR= interquartile range; MHI = median household income; LOS= length of stay.
DM = diabetes; IQR= interquartile range; MHI = median household income; LOS= length of stay.Patient Location: 1- Central counties of metro areas of >=1 M population; 2- Fringe counties of metro areas of >=1 million population; 3- Counties in metro areas of 250,000-999,999 population; 4- Counties in metro areas of 50,000-249,999 population; 5- Micropolitan counties; 6- Not metropolitan or micropolitan counties
Table 2. Logistic regression analyses showing adjusted odds of hospitalization of children with diabetes and asthma during 2016 and 2019
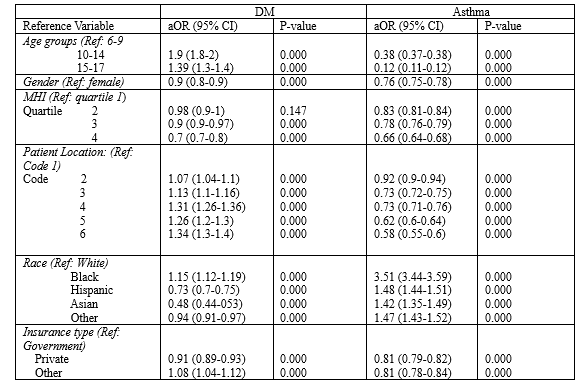 OR= Odds Ratio; Patient location:: 1- Central counties of metro areas of >=1 M population; 2- Fringe counties of metro areas of >=1 million population; 3- Counties in metro areas of 250,000-999,999 population; 4- Counties in metro areas of 50,000-249,999 population; 5- Micropolitan counties; 6- Not metropolitan or micropolitan counties
OR= Odds Ratio; Patient location:: 1- Central counties of metro areas of >=1 M population; 2- Fringe counties of metro areas of >=1 million population; 3- Counties in metro areas of 250,000-999,999 population; 4- Counties in metro areas of 50,000-249,999 population; 5- Micropolitan counties; 6- Not metropolitan or micropolitan countiesForest plot depicting adjusted odds of hospitalization of children with diabetes and asthma income quartiles 2-4 compared to 1st quartile.