Emergency Medicine 12
Session: Emergency Medicine 12
548 - The Effects of Emergency Department Overcrowding on Trauma Response Times
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 548.6966
Branae Rollins, Children's Hospital Los Angeles, Los Angeles, CA, United States; Alice M. Martino, University of California, Irvine, School of Medicine, Orange, CA, United States; Natalie F. Glassman, Children's Hospital Los Angeles, Los Angeles, CA, United States; Shadassa Ourshalimian, Children's Hospital Los Angeles, Los Angeles, CA, United States; Pradip P. Chaudhari, Children's Hospital Los Angeles, Los Angeles, CA, United States; Ryan Spurrier, Children's Hospital Los Angeles, Hermosa Beach, CA, United States

Branae Rollins, MD
Research Fellow
Children's Hospital Los Angeles
Los Angeles, California, United States
Presenting Author(s)
Background: Emergency department (ED) overcrowding is known to delay patient care and affect outcomes. The National Emergency Department Overcrowding Scale (NEDOCS) is a scoring system used to quantify overcrowding, accounting for the capacity of the ED, the total number of ED patients, the acuity of the patients, and the capacity of the hospital. Although trauma team response time is a key metric for trauma center accreditation, the impact of ED response times on trauma care has not been well studied.
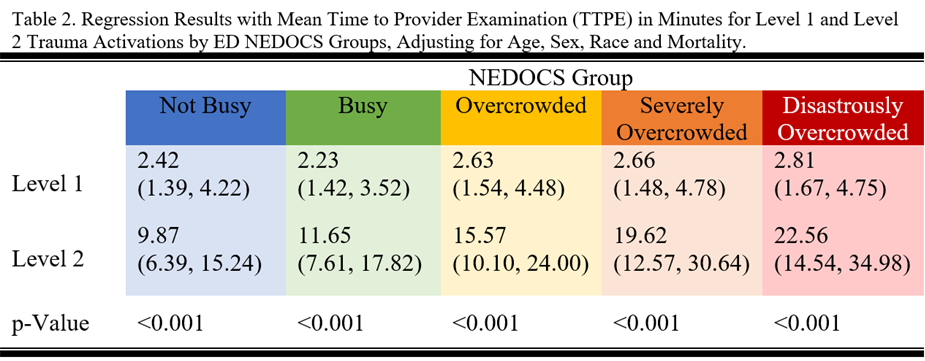
Objective: We hypothesize that while level 1 trauma response times will be consistent across all NEDOCS groups, the provider response time for level 2 trauma activations will increase with increasing ED busyness.
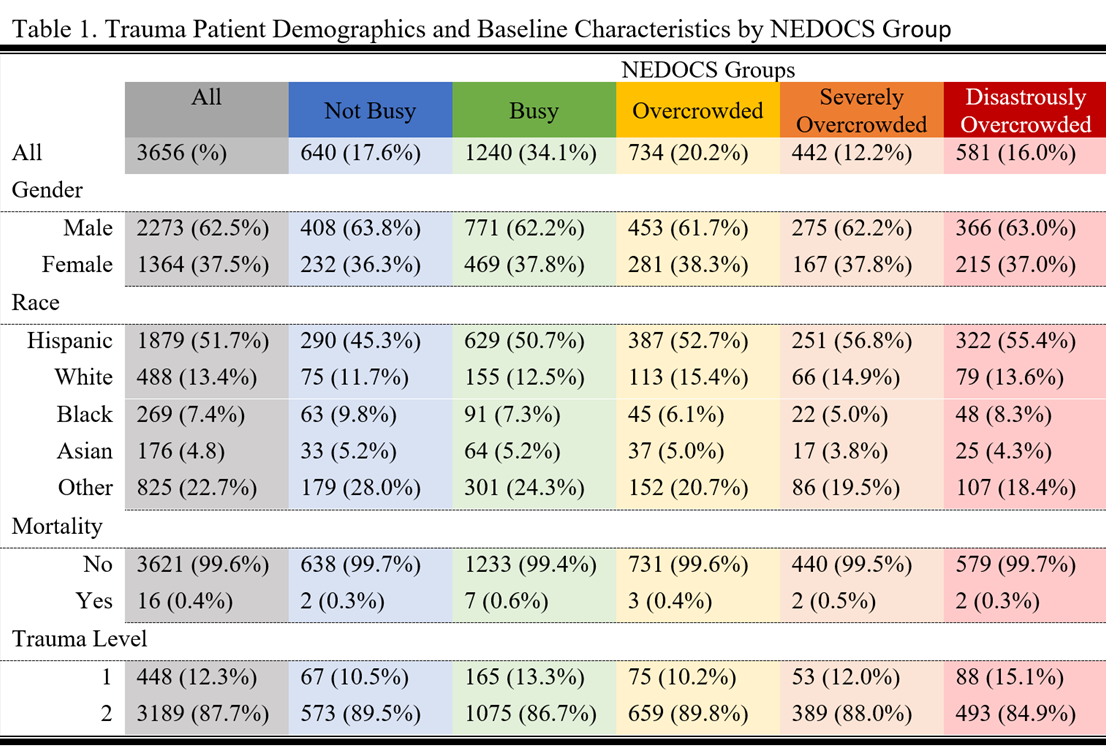
Design/Methods: This retrospective observational study was conducted at Children's Hospital of Los Angeles from January 2016 to December 2022, analyzing 3,656 trauma patients. NEDOCS scores at patient arrival were used to categorize ED crowding into five groups: Not Busy (0-50), Busy (51-100), Overcrowded (101-140), Severely Overcrowded (140-180), and Disastrously Overcrowded (>180). Time to provider examination (TTPE) was compared between level 1 and level 2 trauma activations within each NEDOCS category using log-linear regression models, adjusting for patient characteristics.
Results: Overall, most patients were male (62.2%), predominantly Hispanic (51.7%), and considered as level 2 trauma activations (87.7%). Mortality was rare (0.4%). On adjusted regression results, the estimated mean TTPE for level 1 traumas was consistently around 2 minutes across NEDOCS groups, demonstrating no significant delays despite increasing ED crowding. Conversely, mean TTPE for level 2 traumas increased with higher crowding levels: from 9.87 (6.39-15.24; 95% CL) minutes in the Not Busy group to 22.56 (14.54-34.98; 95% CL) minutes in the Disastrously Overcrowded group. In the disastrously overcrowded group, the TTPE for level 2 traumas was 8.02 times longer when compared to the level 1 response times.
Conclusion(s): Emergency Department overcrowding led to significant delays in level 2 trauma response times, while level 1 trauma response times remained unaffected across all levels of crowding. These findings highlight an opportunity for improvement in the current trauma response, particularly for lower-priority trauma cases, as crowding escalates. Addressing such delays could optimize trauma care and patient outcomes, especially under high-demand conditions. Future research should focus on identifying leverage points that contribute to delays, such as triage inefficiencies or missed activation criteria.