Children with Chronic Conditions 3
Session: Children with Chronic Conditions 3
467 - Training Students as Navigators for a Community-Clinical Linkage Model to Improve Access to School-Based Therapies
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 467.6975
Karis M. Gorak, University of Illinois College of Medicine, Chicago, IL, United States; Tina L. Schuh, University of Illinois College of Medicine, Chicago, IL, United States; Reshma Shah, University of Illinois Chicago, Chicago, IL, United States
.jpg)
Karis M. Gorak, MS, MEd (she/her/hers)
MD/PhD Trainee
University of Illinois College of Medicine
Chicago, Illinois, United States
Presenting Author(s)
Background: Societal inequities create disparities in access to therapies across medical and educational systems, affecting health outcomes for Black, Latino/a/e, and low-income preschool-age children with developmental delays and disabilities (PCw/DD). Community-clinical linkages (CCLs) are a proven strategy to increase access to health-promoting services and may address these disparities. Patient navigators (PNs) support families in connecting with essential services, and student volunteers as PNs provide a valuable resource in academic-affiliated clinics with limited resources. However, effective training resources for students to connect families with PCw/DD to school-based services are limited.
Objective: This study examined the feasibility, acceptability, and initial effectiveness of a protocol to train university-based student volunteers as PNs in a CCL to connect clinics serving historically marginalized communities with early childhood special education (ECSE) services for PCw/DD. We aimed to 1) assess the training’s acceptability to students, 2) determine its impact on student knowledge and self-efficacy, and 3) evaluate PN outreach to families in need of ECSE services.
Design/Methods: Training used group-based, active learning techniques to teach core content (e.g., therapies, health equity) and critical PN skills (e.g., communication, modeling). PN skills were assessed using fidelity checklists during training and family interactions. PNs completed anonymous questionnaires to evaluate training acceptability and self-efficacy (7-point Likert scale) and a knowledge test pre- and post-training. In a hybrid implementation-effectiveness randomized control trial (RCT), we tracked the number of families successfully connected to PNs from those referred.
Results: Thirty-three students applied to the PN training; 13 were selected and 12 completed training (average of 9.5 hours, virtual and in-person across three cohorts). Student satisfaction was high (M=6.42, SD=0.5). Self-efficacy scores rose post-training (Mean 3.5 (1.7) to 5.7 (0.8); p< 0.001), and knowledge significantly increased (Mean 41.4% (0.2) to 93.3% (0.1); p< 0.001; see Table 1). Of 125 enrolled families from March to October 2024, 63 were randomized to receive PN services. PNs reached 98% (n=62) of families with 99% protocol fidelity.
Conclusion(s): These results suggest use of this training protocol may be a feasible way to train student volunteers to serve as PN to in CCLs models, particularly in academic settings with limited resources. Future studies should examine protocol use in other clinical settings and parental perceptions of PNs.
Table 1
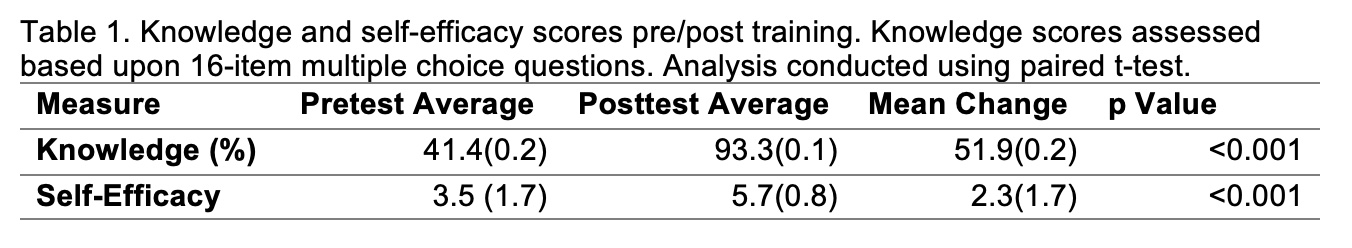 Knowledge and self-efficacy scores pre/post training. Knowledge scores assessed based upon 16-item multiple choice questions. Analysis conducted using paired t-test.
Knowledge and self-efficacy scores pre/post training. Knowledge scores assessed based upon 16-item multiple choice questions. Analysis conducted using paired t-test. 
