Neonatal Neurology 7: Pre-Clinical 1
Session: Neonatal Neurology 7: Pre-Clinical 1
5 - Lack of additional benefit from slow rewarming after therapeutic hypothermia for ischemic brain injury in near-term fetal sheep
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 5.5812
Alice McDouall, The University of Auckland, Auckland, Auckland, New Zealand; Kelly Zhou, University of Auckland, Auckland, Auckland, New Zealand; Guido Wassink, University of auckland, Auckland, Auckland, New Zealand; Anthony L. Davies, The University of Auckland, Auckland, Auckland, New Zealand; Laura Bennet, The University of Auckland, Auckland, Auckland, New Zealand; Alistair J.. Gunn, The University of Auckland, Auckland, Auckland, New Zealand; Joanne Davidson, The University of Auckland, Auckland, Auckland, New Zealand

Joanne Davidson, PhD (she/her/hers)
Associate Professor
The University of Auckland
Auckland, Auckland, New Zealand
Presenting Author(s)
Background: The optimal rate of rewarming after therapeutic hypothermia is unclear. Speculatively, slow rewarming is thought to reduce cardiovascular instability and rebound seizures, but there is little controlled evidence to support this.
Objective: This study investigated whether slow rewarming could improve neuroprotection after 72 h of hypothermia.
Design/Methods: Term-equivalent fetal sheep (0.85 gestation) received sham occlusion (n=8) or 30 minutes of global cerebral ischemia followed by normothermia (n=7), or hypothermia from 3-72 h with either fast, spontaneous rewarming within 1 h (n=8) or slow rewarming at 0.5 °C/h over 10 h (n=8).
Results: Hypothermia improved electroencephalogram (EEG) and spectral edge recovery (P < 0.05), with no significant difference between fast and slow rewarming (Figure 1, P>0.05). Hypothermia reduced the number of seizures (P < 0.05), with no significant difference in seizure activity during or after hypothermia between fast and slow rewarming (P>0.05). Hypothermia improved neuronal survival in the cortex, cornu ammonis (CA)1, CA3, CA4 and dentate gyrus regions of the hippocampus (P < 0.05), with no significant difference between fast and slow rewarming (P>0.05). Hypothermia attenuated microglial number in the cortex (P < 0.05), with no significant difference between fast and slow rewarming (P>0.05).
Conclusion(s): The rate of rewarming after a clinically relevant duration of hypothermia had no effect on neurophysiological recovery, neuronal survival or number of microglia after global cerebral ischemia in term-equivalent fetal sheep. Reassuringly, the rate of rewarming had no effect on rebound seizure activity during or after rewarming.
Change in EEG power, spectral edge frequency and impedance before, during and after 30 min of ischemia (time 0) in the sham control, ischemia-normothermia, ischemia-hypothermia fast rewarming and ischemia-hypothermia slow rewarming groups.
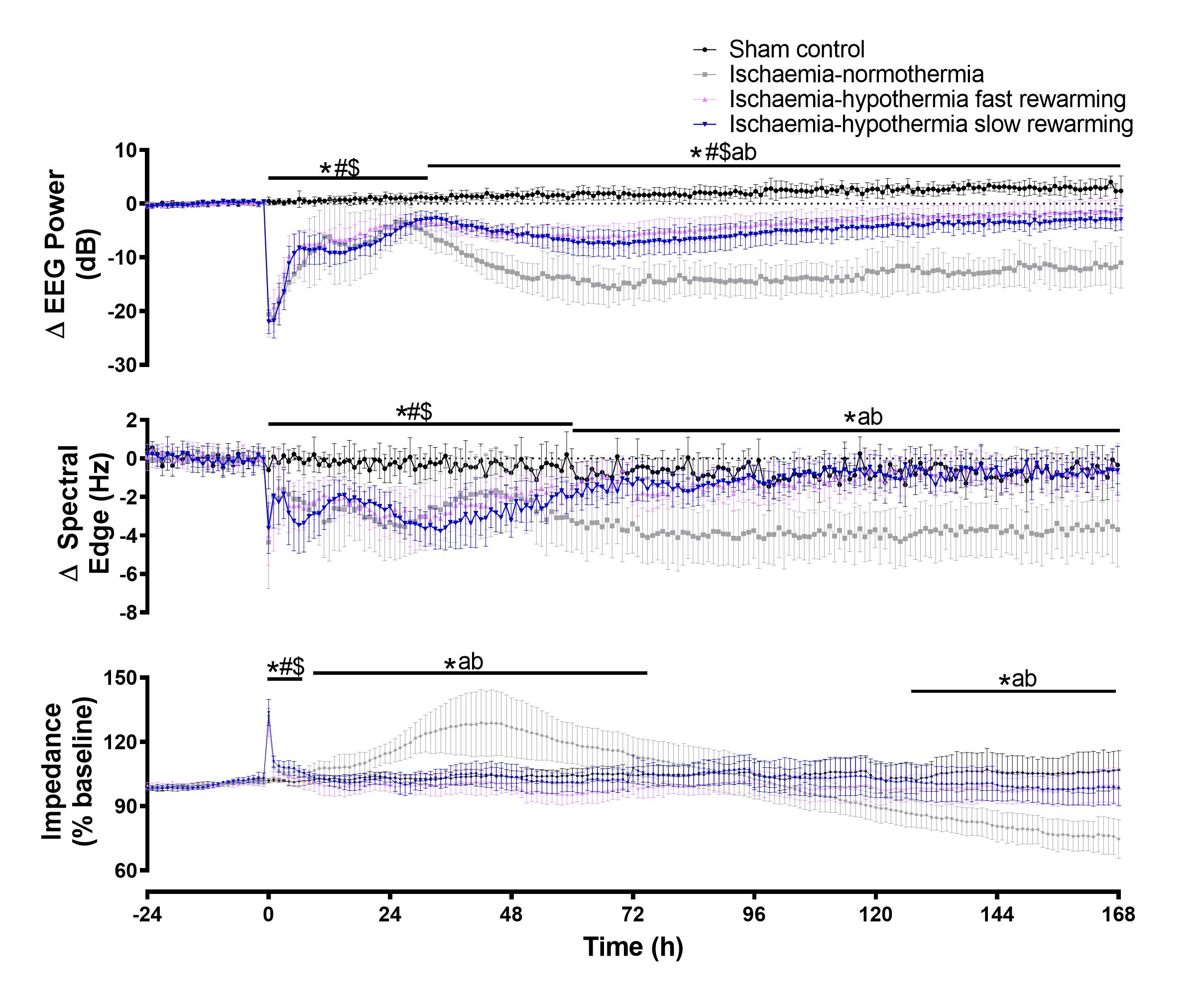 The rate of rewarming was not associated with any difference in recovery of EEG power, spectral edge frequency or cell swelling (impedance). * P<0.05 sham control vs. ischemia-normothermia, # P<0.05 sham control vs. ischemia-hypothermia fast rewarming, $ P<0.05 sham-control vs. ischemia-hypothermia slow rewarming, a P <0.05 ischemia-normothermia vs. ischemia-hypothermia fast rewarming, b P<0.05 ischemia-normothermia vs. ischemia-hypothermia slow rewarming.
The rate of rewarming was not associated with any difference in recovery of EEG power, spectral edge frequency or cell swelling (impedance). * P<0.05 sham control vs. ischemia-normothermia, # P<0.05 sham control vs. ischemia-hypothermia fast rewarming, $ P<0.05 sham-control vs. ischemia-hypothermia slow rewarming, a P <0.05 ischemia-normothermia vs. ischemia-hypothermia fast rewarming, b P<0.05 ischemia-normothermia vs. ischemia-hypothermia slow rewarming.
