Neonatal General 11
Session: Neonatal General 11
413 - Successful placement of umbilical arterial and venous catheter and prognosis in congenital diaphragmatic hernia
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 413.6922
Satyan Lakshminrusimha, UC Davis, Sacramento, CA, United States; Elva Horath, University of California Davis Children's Hospital, Citrus Heights, CA, United States; Stanley Smith, UC Davis Children's Hospital, Sacramento, CA, United States; Evan M. Giusto, UC Davis Health, Sacramento, CA, United States

Elva Horath, MD (she/her/hers)
Pediatric Telehealth Project Policy Analyst
University of California Davis Children's Hospital
Citrus Heights, California, United States
Presenting Author(s)
Background: Congenital diaphragmatic hernia (CDH) is associated with high morbidity, prolonged length of stay, and high mortality (~ 25-30%). Herniation of the liver into the thoracic cavity and distorted anatomy of ductus venosus and inferior vena cava may be associated with CDH. Patency of the ductus venosus is needed for successful umbilical venous catheter (UVC) placement.
Objective: Evaluation of successful cannulation with proper positioning of umbilical lines in neonates born with congenital diaphragmatic hernia
Design/Methods: This is a single center, retrospective analysis of CDH patients. The following data were compared between patients with and without successful umbilical line placement.
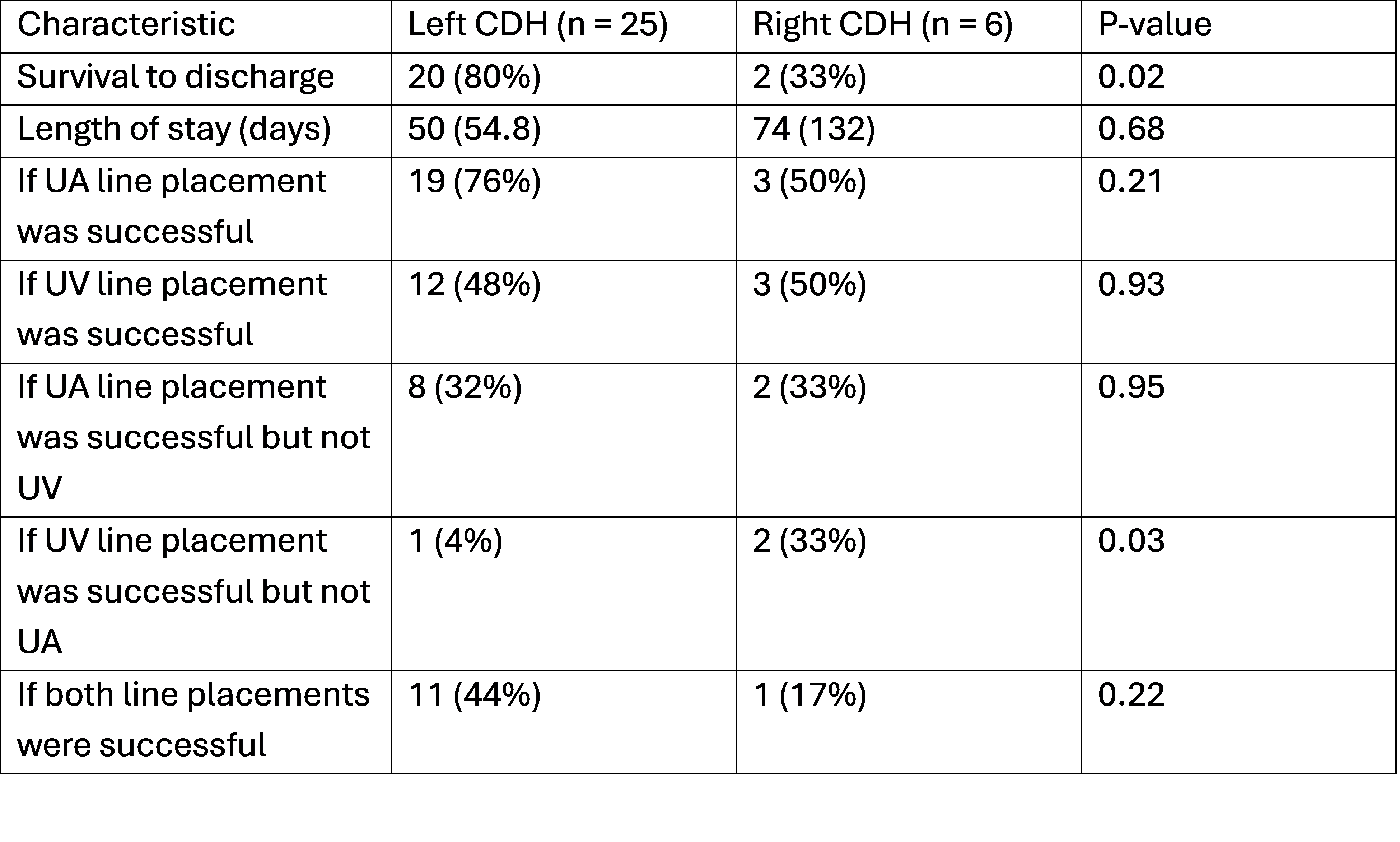
Results: 31 infants with CDH were admitted during the study period of 2019-2024. Placement of umbilical arterial (UAC) and UVC both were successful only in 12 (37.5%). UAC placement was successful in 22 (69%) and UVC in 15 (47%). There was a tendency towards higher need for pulmonary vasodilators, vasopressors, mortality before discharge, and longer length of stay when placement of UAC+UVC was not successful (Table 1). In a sub-analysis of UVC placement, there continued to be a tendency towards a higher need for pulmonary vasodilators, vasopressors, and mortality (Table 2). While right CDH had a higher mortality rate, there was no difference in successful umbilical line placement between left and right CDH (Table 3).
Conclusion(s): In a level IV NICU, UVC could not be placed in more than half of CDH patients. Backup plans for a quick PICC /central line placement should be readily available following the admission of patients CDH with unsuccessful UVC placement, as there is a higher need for vasopressor support amongst these patients.
Table 1: Characteristics between Successful and Unsuccessful Umbilical Line Placement
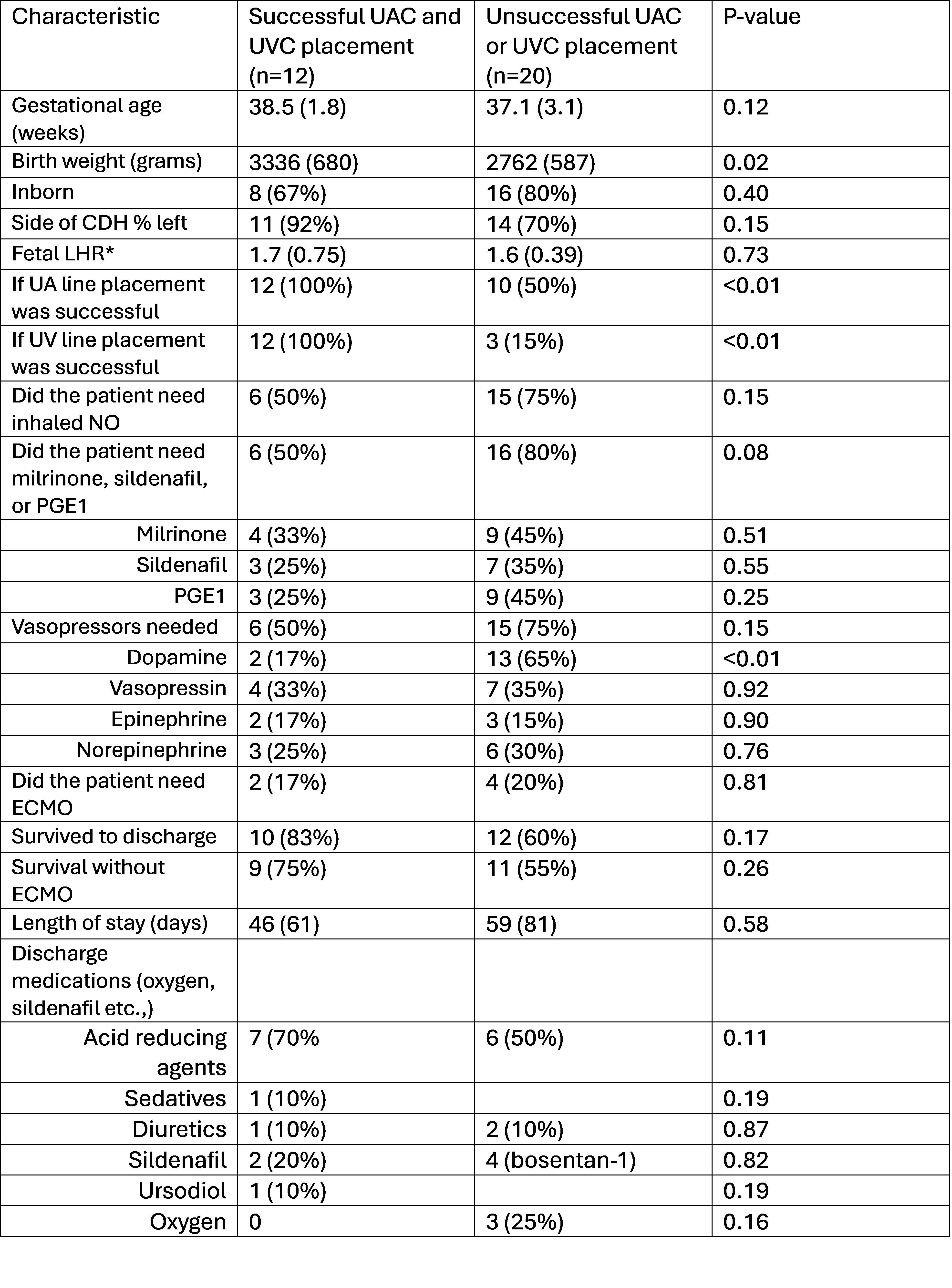 *Fetal LHR data only available 12 patients (6 in each group)
*Fetal LHR data only available 12 patients (6 in each group)P-value = unpaired t-test for continuous values or chi-square test for dichotomous characteristics
Table 2: Comparison of Characteristics of Central Umbilical Venous Catheter Placement
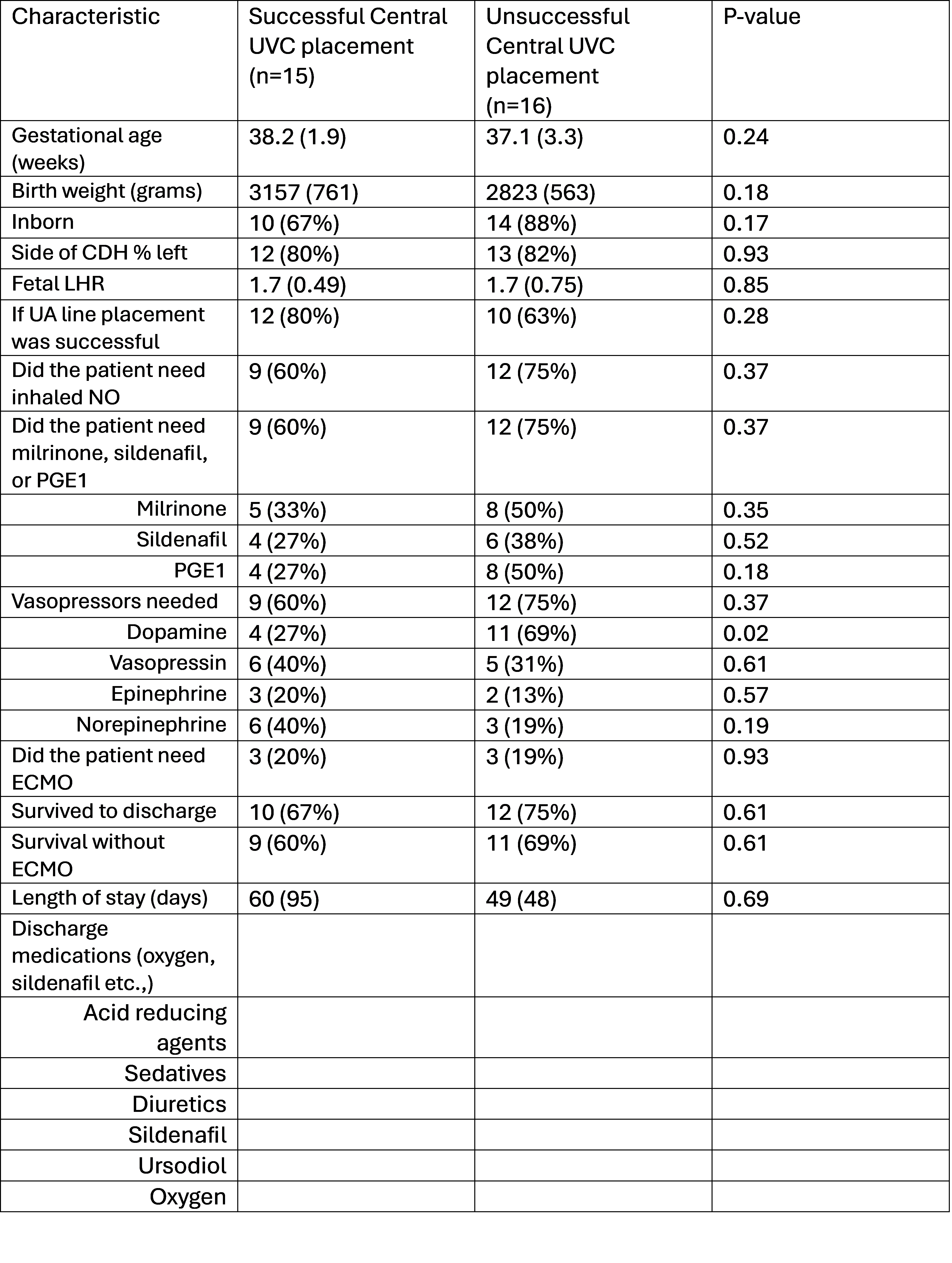 *Fetal LHR data only available 12 patients (6 in each group)
*Fetal LHR data only available 12 patients (6 in each group)P-value = unpaired t-test for continuous values or chi-square test for dichotomous characteristics
Table 3: Comparison of Left vs Right CDH