Neonatal/Infant Resuscitation 3
Session: Neonatal/Infant Resuscitation 3
390 - Variations in practices at birth of preterm neonates among neonatal units of 12 population-based national or regional neonatal networks
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 390.7056
Maria Fernanda de Almeida, Universidade Federal de Sao Paulo, Sao Paulo, Sao Paulo, Brazil; Ruth Guinsburg, Universidade Federal de São Paulo, São Paulo, Sao Paulo, Brazil; Kjell Helenius, University of Turku, Turku, Varsinais-Suomi, Finland; Neha Goswami, Mount Sinai Hospital, Toronto, ON, Canada; Maximo Vento, Instituto de Investigación Sanitaria La Fe, VALENCIA, Comunidad Valenciana, Spain; Valerie Biran, Robert Debre Children's Hospital, Assistance Publique Hôpitaux de Paris,Université Paris-Cité, INSERM U1141, France, Paris, Ile-de-France, France; Tomasz Szczapa, II Department of Neonatology, Poznan University of Medical Sciences (PUMS), Poznan, Wielkopolskie, Poland; Malcolm Battin, Auckland City Hospitial, Auckland, Auckland, New Zealand; Satoshi Kusuda, Neonatal Research Network of Japan, Taito, Tokyo, Japan; Mikael Norman, Karolinska Institutet, Stockholm, Stockholms Lan, Sweden; Simone Pratesi, University of Florence, Florence, Toscana, Italy; Mark Adams, University Hospital Zurich, Zurich, Zurich, Switzerland; Dirk Bassler, University Hospital of Zurich, Zurich, Zurich, Switzerland; Kei Lui, University of New South Wales, Sydney, New South Wales, Australia; Laura San Feliciano, Hospital Universitario de Salamanca, Salamanca, Castilla y Leon, Spain; Liisa Lehtonen, University of Turku, Turku, Varsinais-Suomi, Finland; Gil Klinger, Schneider Children's Medical Center of Israel and Tel Aviv University, Ramat Hasharon, HaMerkaz, Israel; Tetsuya Isayama, National Center for Child Health and Development, Setagaya-ku, Tokyo, Japan; Brian Reichman, Sheba Medical Center, Ramat Gan, HaMerkaz, Israel; Marc Beltempo, McGill University Faculty of Medicine and Health Sciences, Monreal, PQ, Canada; Prakesh S. Shah, Mount Sinai Hospital, Toronto, ON, Canada
.jpg)
Maria Fernanda Branco de Almeida, MD, PhD (she/her/hers)
Associate Professor
Universidade Federal de São Paulo
São Paulo, Sao Paulo, Brazil
Presenting Author(s)
Background: Although neonatal resuscitation guidelines are based on international scientific consensus and treatment recommendations periodically updated, variations in their application and integration into daily practice may occur.
Objective: To survey the variations in practices at birth of preterm neonates of < 29 weeks’ gestation among neonatal units of 12 population-based national or regional neonatal networks participating in the International Network for Evaluating Outcomes in Neonates (iNeo).
Design/Methods: Online pre-piloted questionnaires were sent to the directors of 608 NICU’s participating in Australia/New-Zealand (ANZNN n= 30), Brazil (RBPN n=20), Canada (CNN, n=32), Finland (FinMBR, n=5), France (FR, n=70), Israel (INN, n=26), Japan (NRNJ, n=292), Poland (PL, n=56), Spain (SEN1500, n=55), Sweden (SNQ n=9), Switzerland (SwissNeoNet n=9), and Tuscany, Italy (TuscanNN n=4). The responses based on practices in 2023 were reported as frequency of units in each network.
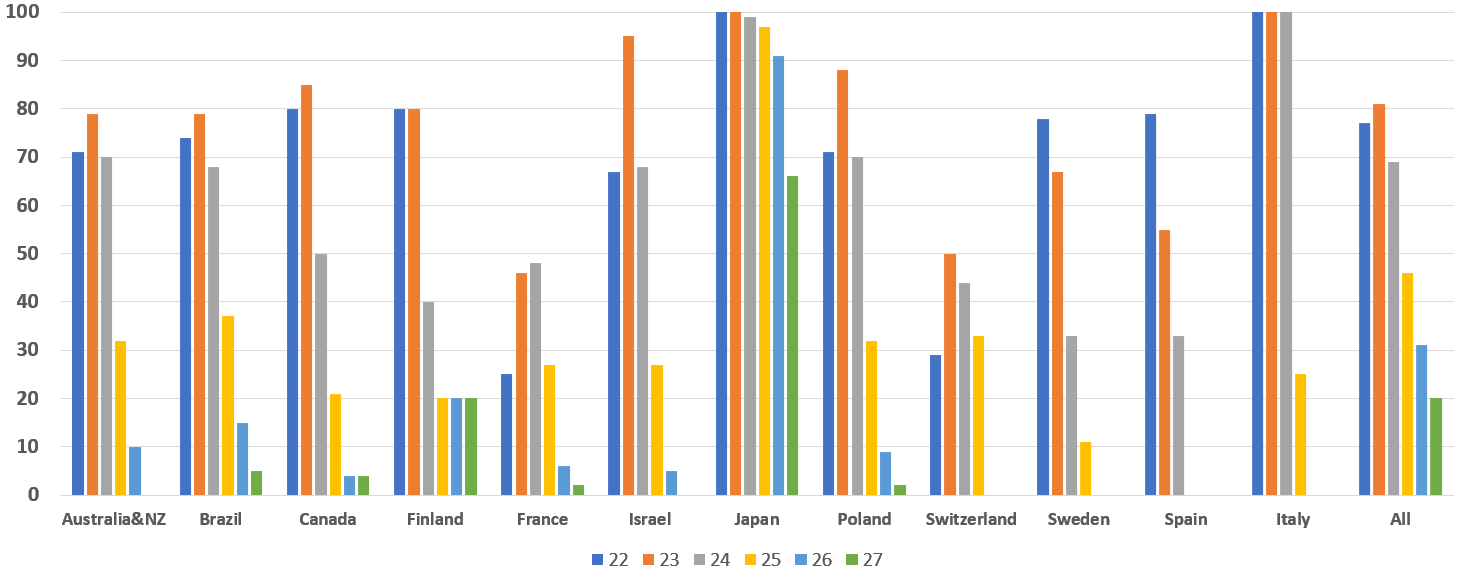
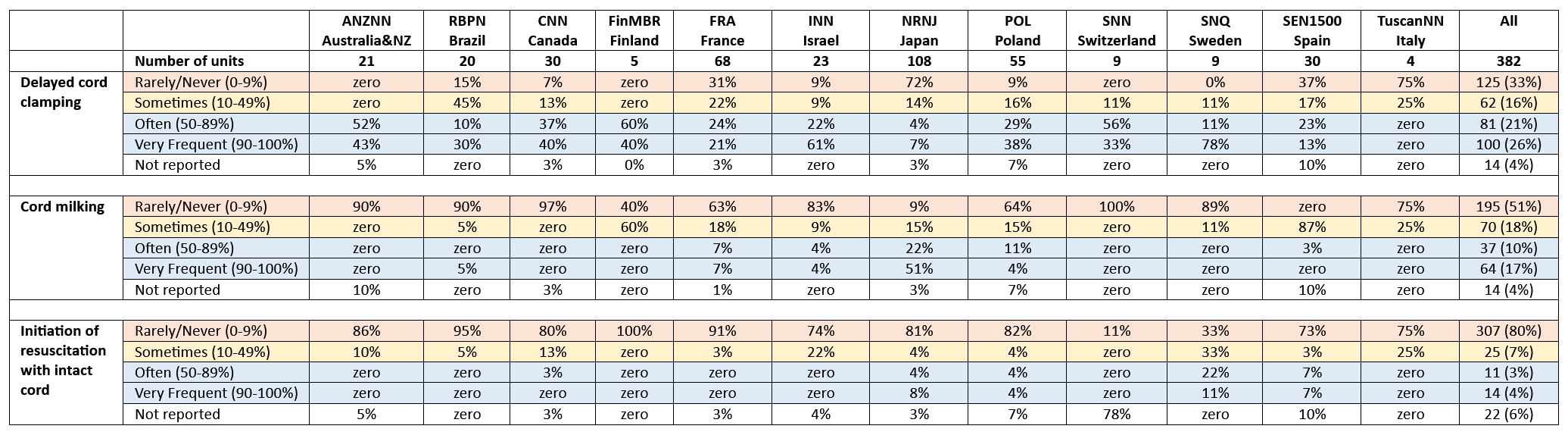
Results: Overall, 382 units (63%) responded the survey, varying from 37-100% among networks. Active resuscitation at 22, 23 and 24 weeks gestation at birth was often/very frequently offered, respectively, by 19%, 48% and 70% of units, with wide networks’ variation (Table 1). Delayed cord clamping, cord milking and resuscitation with intact cord were often/very frequently offered to infants < 28 weeks in, respectively, 47%, 27% and 7% of the 382 units. Japan contributed with 80% of the units reporting often/very frequent cord milking (Table 2). Written guidelines to avoid hypothermia were referred by 73% of the 382 units. Use of warm towel (59%), plastic wrap (75%), preheated warmer (71%), thermal mattress (38%) and heated gases (31%) varied across networks. Only in Sweden ≥80% units adopted all thermal care procedures at birth. Tracheal tube as the preferred interface for ventilatory support at birth decreased as gestational age increased. For infants born at 27-28 weeks, preference for intubation at birth was rare across networks, except for Japan (Figure). Routine prophylactic surfactant in the delivery room was reported by 24% of the 382 units, varying from zero (Brazil) to 40% (Finland). Initial O2 concentration < 40% for respiratory support at birth was reported by 86% of the 382 units.
Conclusion(s): There were marked variations in the delivery room management of very preterm infants between networks. Enhanced collaboration is needed, with a focus on implementing international recommendations for neonatal care at birth across countries and units.
Table 1. Proportion of units in each network that answered on the frequency that live births without major congenital anomaly receive active resuscitation at birth, according to gestational age (GA) in weeks (wk)
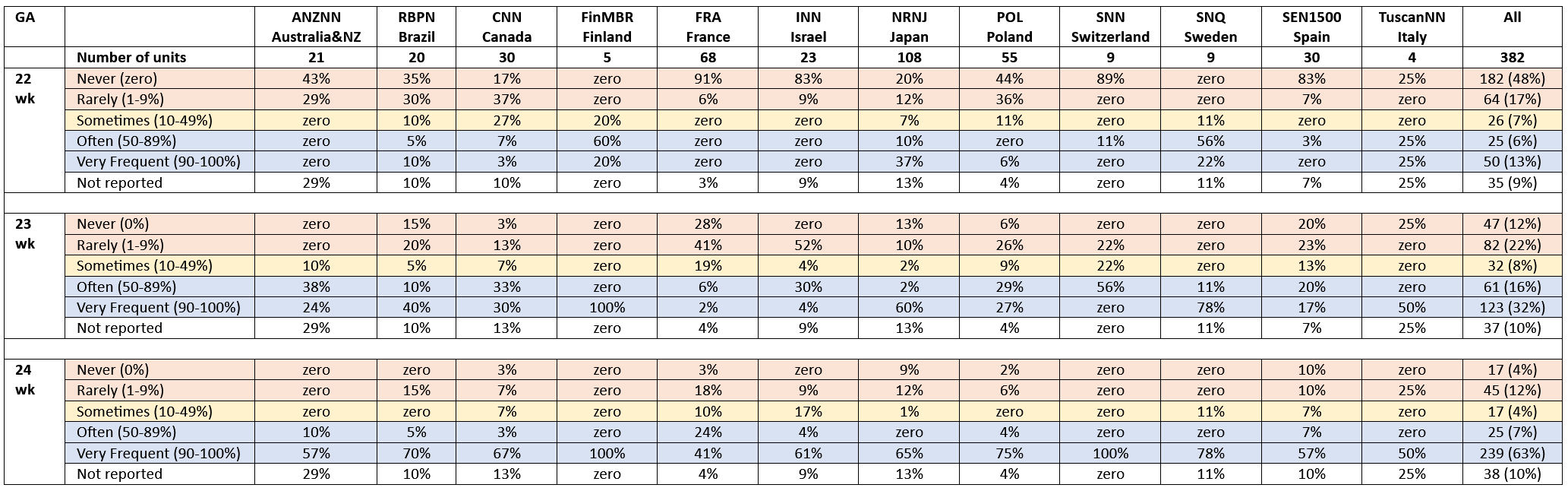
Table 2. Proportion (%) of units in each network that answered on the frequency of different strategies on umbilical cord management in preterm infants <28 weeks gestation
Proportion (%) of units in each network that reported endotracheal intubation as the initial preferred interface for respiratory support in the majority (>60%) of neonates in the delivery room, according to gestational age (GA) in weeks (wk).