Neonatal General 12: Prenatal Exposures
Session: Neonatal General 12: Prenatal Exposures
434 - Nasogastric and orogastric tube feeding among infants with intrauterine opioid exposure
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 434.5611
Margarida Mascarenhas, Holtz Children's Hospital Jackson Memorial Hospital, Miami, FL, United States; Leslie Kerzner, Harvard Medical School, Lynnfield, MA, United States; Leela Sarathy, Mass General for Children, Boston, MA, United States; Elisha M. Wachman, Boston University School of Medicine, Boston, MA, United States; Davida Schiff, Massachusetts General Hospital, Boston, MA, United States
.jpg)
Margarida Mascarenhas, MD, MMSc (she/her/hers)
Pediatrics Resident
Holtz Children's Hospital - Jackson Memorial Hospital
Miami, Florida, United States
Presenting Author(s)
Background: Intrauterine opioid exposure (IOE) can contribute to increased energy expenditure and negatively affect neonatal oral feeding leading to excessive neonatal weight loss. Nasogastric (NG) or orogastric (OG) tube feedings may be necessary to provide adequate nutrition and minimize neonatal weight loss. The prevalence and factors associated with infants with IOE requiring tube feeding remain unknown.
Objective: To describe the prevalence and duration of NG or OG tube feeding among infants with IOE and examine the extent to which maternal and infant factors are associated with the use of tube feeding.
Design/Methods: We conducted a retrospective cohort study of infants, born after 37 weeks’ gestation, who were observed or treated for Neonatal Opioid Withdrawal Syndrome (NOWS) and received supplemental feeding, at a tertiary care hospital in Massachusetts between 2018-2023. Primary outcomes were any initiation of nasogastric or orogastric feeding and duration of tube feeding. We used stepwise selection and multivariable logistic regression to identify maternal and infant factors associated with tube feeding.
Results: We identified 108 mother-infant dyads with IOE that received supplemental feeding. Mothers were mostly non-Hispanic White (84%) and only on medication for opioid use disorder (MOUD) or other prescribed opioids (61%). Almost half the infants (47%) were treated pharmacologically. Thirty-three infants (30.6%) required tube feeding. Median initiation of tube feeding was on the 2nd day of life (IQR 1-4) and had median duration of 5.5 days (IQR 3-12). Prevalence of tube feeding ranged from 0% to 100% over six-month intervals, with an overall increasing trend. Tube-fed infants were more likely to have prolonged length of stay (aOR 1.09, CI 1.04-1.13), to have respiratory distress (aOR 12.59, CI 3.1-50.7) and to have been exposed to only non-prescribed opioids in utero (aOR 21.19, CI 2.0-223.4).
Conclusion(s): In a cohort of infants with IOE, 31% required NG or OG tube feeding during their newborn hospitalization, with increasing trends over the study period. The majority of tube feeds were initiated in the first two days of life and lasted under one week. Tube-fed infants were more likely to be have prolonged length of stay, respiratory distress and be exposed to only non-prescribed opioids in utero. Further research is needed to understand the etiologies of feeding difficulties, including the role of exposure to non-prescribed opioids and varying trends over time.
Figure 1. Prevalence of infants requiring nasogastric/orogastric feeds
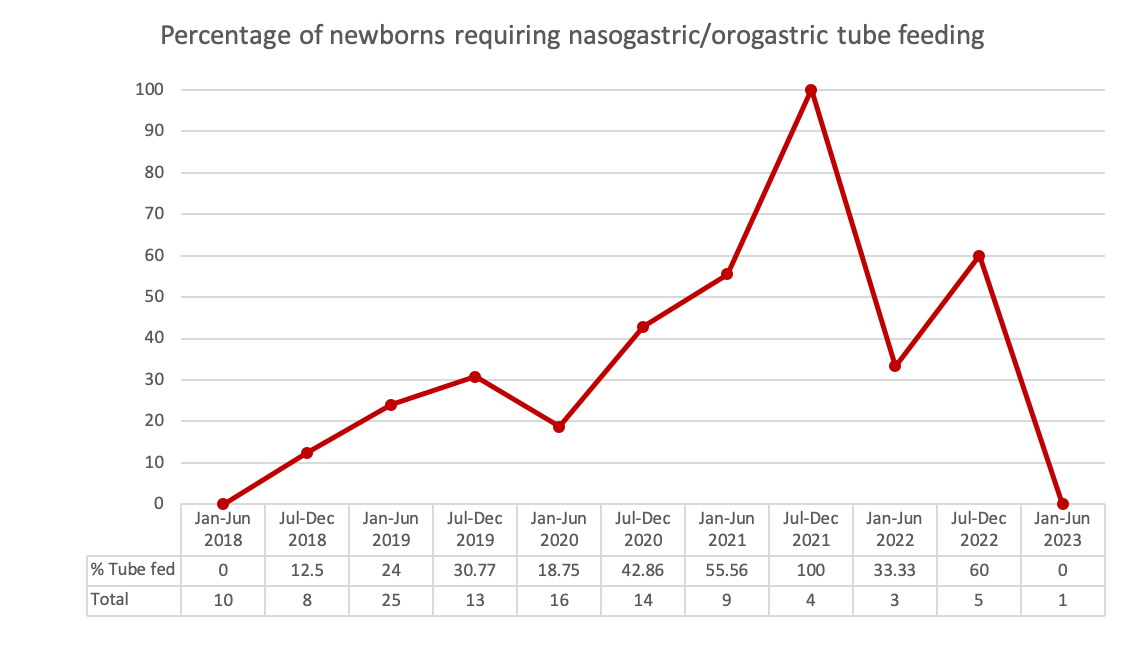
Table 1. Characteristics of the cohort by need for nasogastric/orogastric tube feeding
.jpg)
Figure 2. Multivariable logistic regression for need for nasogastric/orogastric tube feeding
.jpg)
Figure 1. Prevalence of infants requiring nasogastric/orogastric feeds
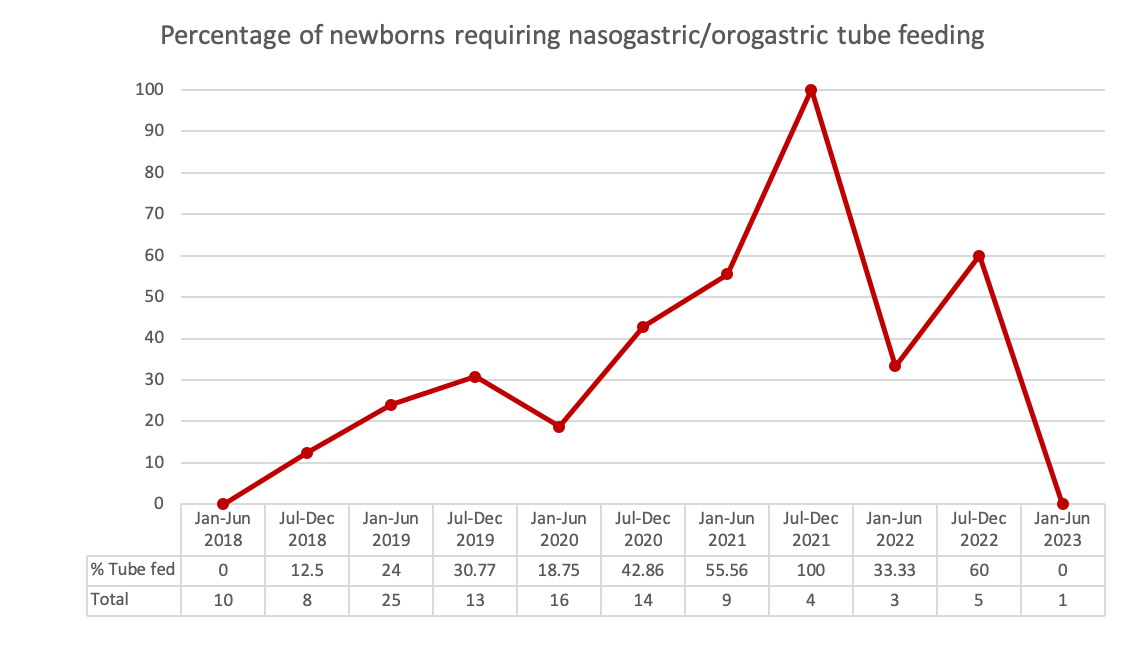
Table 1. Characteristics of the cohort by need for nasogastric/orogastric tube feeding
.jpg)
Figure 2. Multivariable logistic regression for need for nasogastric/orogastric tube feeding
.jpg)

