Neonatal GI Physiology & NEC 4
Session: Neonatal GI Physiology & NEC 4
705 - Heart Rate Variability Metrics in Neonates: Identifying Risk Factors for Necrotizing Enterocolitis
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 705.5546
Joanna Jain, Stanford University School of Medicine, Stanford, CA, United States; Anoop Rao, Lucile Packard Children's Hospital Stanford, Palo ALto, CA, United States

Joanna Jain, B.S. (she/her/hers)
Clinical Research Coordinator Associate
Stanford University School of Medicine
Stanford, California, United States
Presenting Author(s)
Background: Necrotizing enterocolitis (NEC) is an ominous gastrointestinal disease affecting preterm neonates, often leading to severe morbidity and mortality. Heart rate variability (HRV) metrics are potential indicators of autonomic function and may provide insight into the risk of development of NEC.
Objective: To identify predictive HRV metrics for NEC by comparing HRV data from control neonates to those diagnosed with medical (mNEC) and surgical (sNEC) forms of NEC.
Design/Methods: In this Stanford IRB approved study, RR interval data (milliseconds) were collected from a total of 47 neonates classified as controls (32), mNEC (9), and sNEC (6). Custom Python scripts were used to compute HRV metrics. Time domain metrics included Root Mean Square of Successive Differences (RMSSD) and Standard Deviation of NN Intervals (SDNN). Frequency domain metrics include normalized low frequency and high frequency bands (nLF and nHF respectively). Hourly median values were assessed for their variability and trends over time. HRV metrics for control cases were analyzed over an 8-day window randomly chosen between the 2nd and 6th weeks of life. HRV metrics for NEC cases were analyzed within 4 days before and 4 days after the NEC diagnosis. The study employed ROC curve analysis to evaluate the discriminative ability of these HRV metrics to assess their performance in predicting NEC.
Results: Table 1 shows the demographics for all the subjects in the study. The median birth gestational age was 27+2, and the median birth weight was 905 grams. The median age at diagnosis of NEC was 25 days of life. 2 patients with NEC died following diagnosis. The ROC curve analysis revealed that RMSSD had a strong area under the curve (AUC) of 0.80, indicating its potential as a predictor for NEC. Normalized Low Frequency (nLF) also had a good AUC of 0.72. RMSSD is a strong indicator of parasympathetic (vagal) activity. nLF indicates a balance between sympathetic and parasympathetic activity.
Conclusion(s): Altered parasympathetic regulation, reflected by RMSSD, is associated with the development of NEC in neonates. The study highlights the value of monitoring HRV metrics for early identification of neonates at risk for NEC, emphasizing the importance of temporal analysis in understanding the dynamics of HRV changes before and after NEC events. In future work, we aim to expand the analysis to increase the number of cases and analyze mNEC and sNEC separately.
Table 1
.png) Patient demographics.
Patient demographics.Figure 1
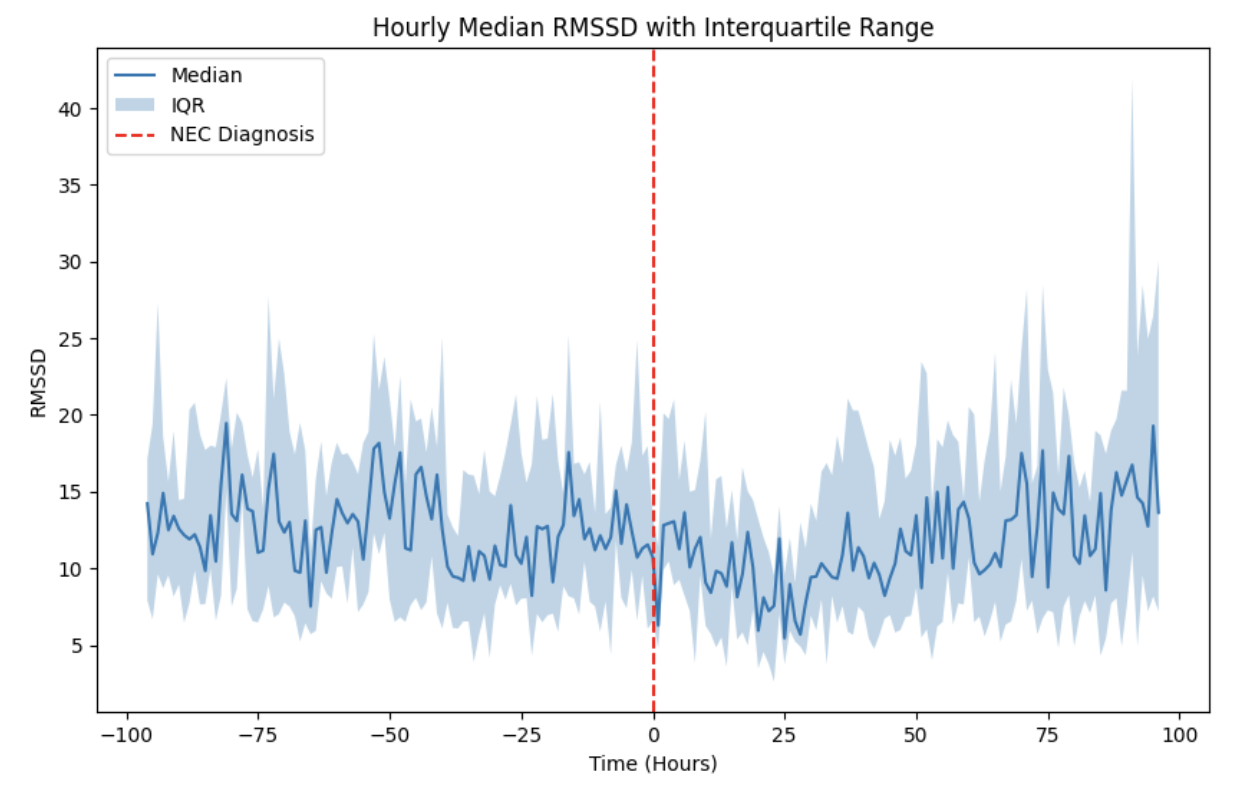 Hourly median RMSSD (in milliseconds) over an 8-day period before and after the diagnosis of medical (mNEC) or surgical NEC (sNEC). The solid blue line represents the median values, while the shaded area indicates the interquartile range (IQR). The dashed red line marks the time of NEC diagnosis.
Hourly median RMSSD (in milliseconds) over an 8-day period before and after the diagnosis of medical (mNEC) or surgical NEC (sNEC). The solid blue line represents the median values, while the shaded area indicates the interquartile range (IQR). The dashed red line marks the time of NEC diagnosis.Figure 2
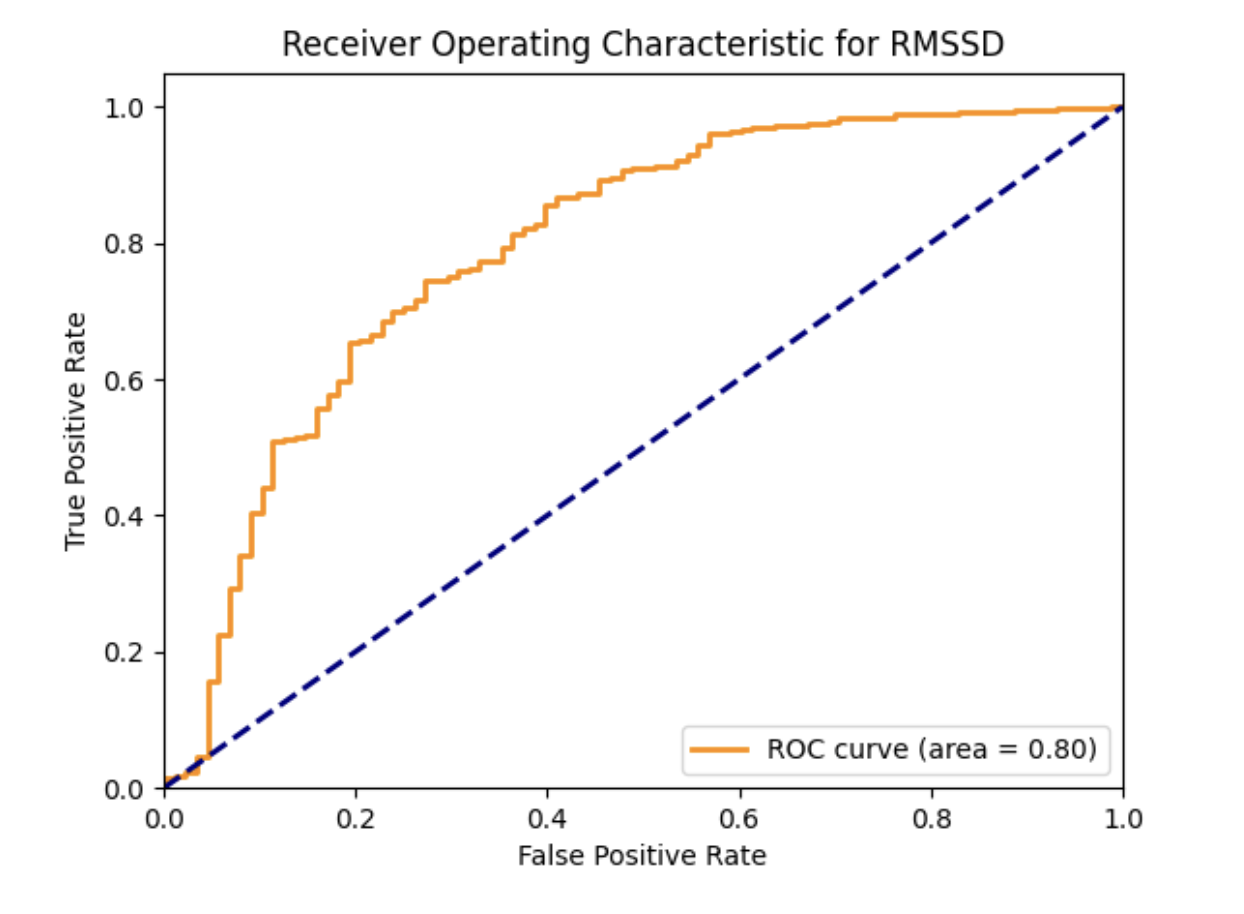 Represents the relationship between the true positive rate (sensitivity) and the false positive rate (1 - specificity) for different thresholds of RMSSD. The area under the ROC curve is 0.80, indicating good discriminatory ability in distinguishing between cases (mNEC and sNEC) and controls. Blue dashed line represents the baseline performance of a random classifier (no discrimination between classes).
Represents the relationship between the true positive rate (sensitivity) and the false positive rate (1 - specificity) for different thresholds of RMSSD. The area under the ROC curve is 0.80, indicating good discriminatory ability in distinguishing between cases (mNEC and sNEC) and controls. Blue dashed line represents the baseline performance of a random classifier (no discrimination between classes).
