Public Health & Prevention 3
Session: Public Health & Prevention 3
781 - Strengthening Wraparound Care for Families with Opioid Use Disorder in the PEDI Clinic Network
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 781.6632
Rafaella Stein Elger, University of South Florida, College of Public Health, Tampa, FL, United States; Amandeep K. Ratta, University of South Florida, Tampa, FL, United States; Chinyere N. Reid, University of South Florida, Tampa, FL, United States; Tara R. Foti, University of South Florida, Tampa, FL, United States; Luiza Mangini, USF Health Morsani College of Medicine, Tampa, FL, United States; Julia Finster, University of Miami Leonard M. Miller School of Medicine, Saint Petersburg, FL, United States; Jennifer Marshall, University of South Florida College of Public Health, Tampa, FL, United States; Tanner Wright, USF Health Morsani College of Medicine, Tampa, FL, United States

Rafaella Stein Elger, MPH, CPH (she/her/hers)
PhD Candidate and Graduate Research Assistant
University of South Florida, College of Public Health
Tampa, Florida, United States
Presenting Author(s)
Background: Young children exposed to opioids in-utero can be at risk for neonatal opioid withdrawal syndrome and neurodevelopmental differences. CADENCE (Continuous and Data-Driven Care) is designed to improve outcomes for children and parents affected by OUD, integrating prenatal, pediatric, addiction medicine, and social support services. Central to CADENCE is the PEDI (Promoting Early Developmental Intervention) clinic, offering multidisciplinary wrap-around stigma-free care prenatally through age five for children and families. In Florida, PEDI plays a key role in supporting children with opioid exposure, mitigating the long-term impacts of social determinants of health surrounding OUD in pregnancy and parenting.
Objective: In this evaluation of PEDI clinic operations and caregivers' experiences, we aimed to identify strengths and areas for improvement through clinical process mapping and examining the clinic’s referral and services networks.
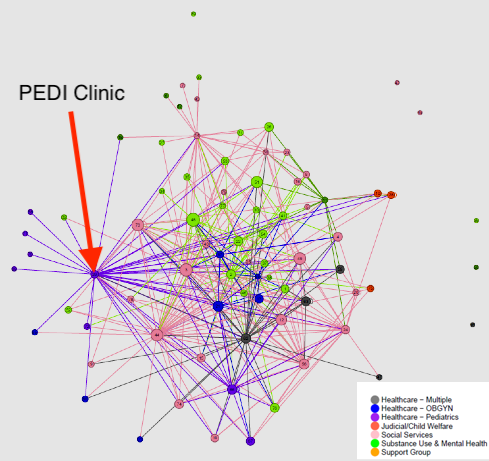
Design/Methods: We used process mapping to understand clinic flow, partner programs, and referral pathways. We conducted clinic observations (n=6), interviews with staff and patients (n=16), CADENCE steering committee meetings/workshops (n=5), and Advisory Group meetings with eight individuals with perinatal OUD) (n=5). Our social network analysis of local agencies (n=78) assessed interagency referrals and collaborations among prenatal, pediatric, office-based opioid therapy clinics, child welfare, early intervention, and other programs.
Results: We identified pathways for patients through process and journey maps, which include referrals, timelines, and access to care (prenatal, pediatric, maternal-fetal medicine, psychiatry). Areas for improvement include streamlining external referrals, enhancing the integration of medications for OUD, reducing stigma, enhancing provider training, improving access to behavioral health care, and lowering financial barriers. Social network maps revealed PEDI's central role in coordinating referrals across service systems, though limited inter-agency relationships were found among some organizations. This emphasizes continuous need for strong interagency communication, coordination, and support for families affected by OUD.
Conclusion(s): Results underscore the complexities that families who have infants and young children face in navigating healthcare systems along with OUD recovery. Family-centered wraparound clinics like PEDI, can connect programs, improve patient retention, and coordinate care to ease burdens and improve health outcomes for these families.
PEDI Clinic flow mapping
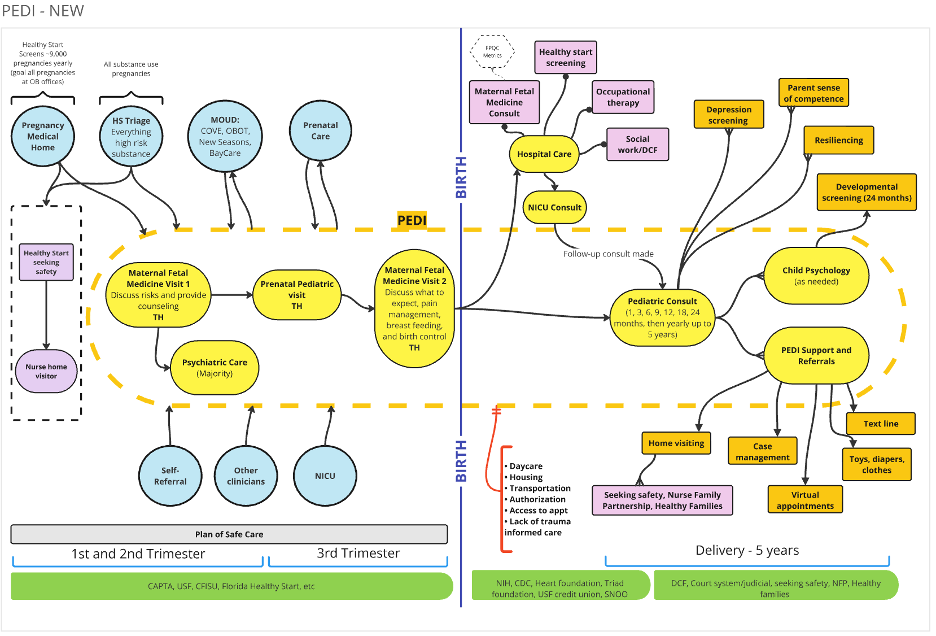 OB: Obstetrician | HS: Hospital | MOUD: Medication for Opioid Use Disorder | TH: Tampa General Hospital | NICU: Neonatal Intensive Care Unit
OB: Obstetrician | HS: Hospital | MOUD: Medication for Opioid Use Disorder | TH: Tampa General Hospital | NICU: Neonatal Intensive Care UnitPatient journey through PEDI Clinic
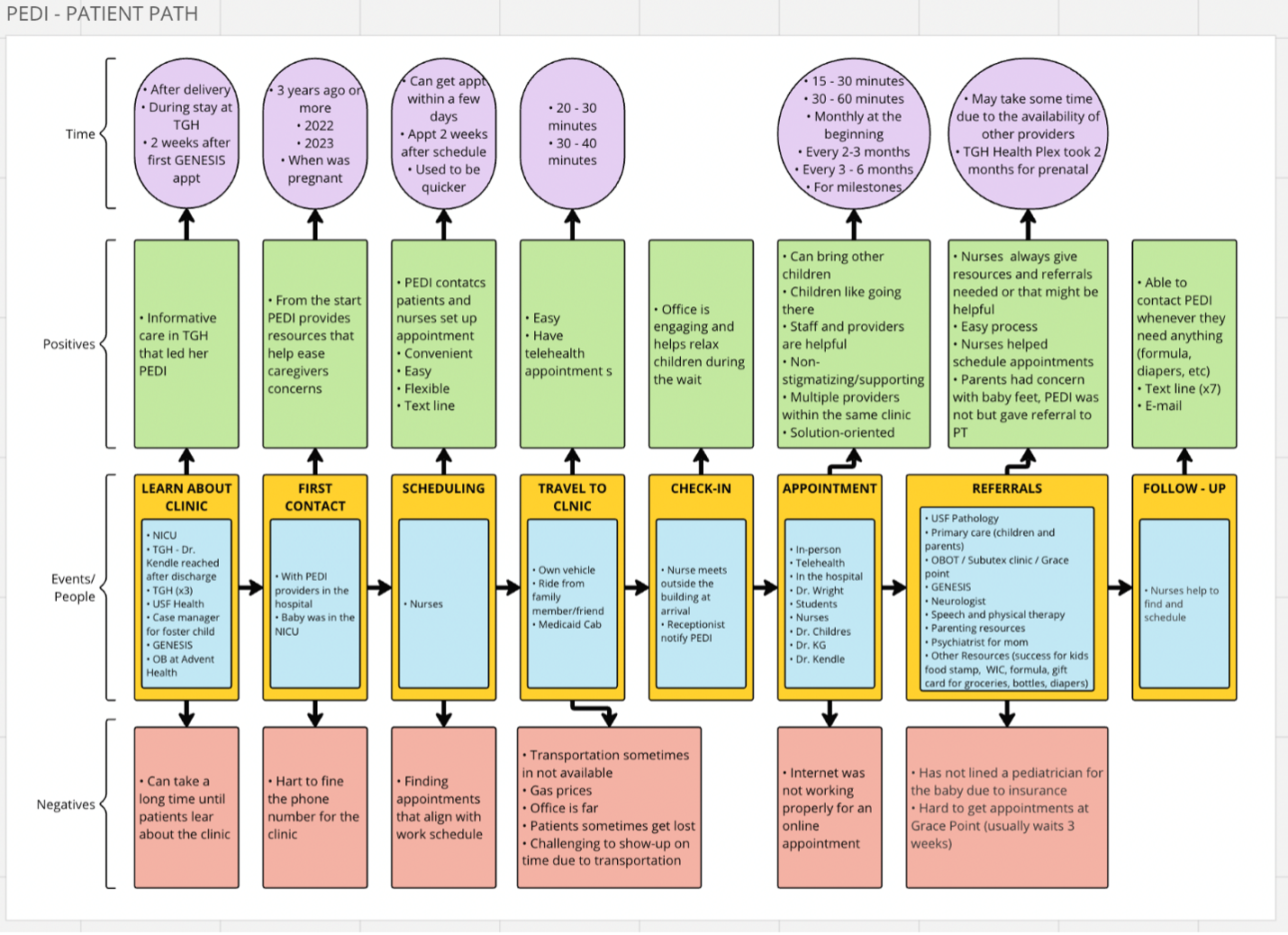 TGH: Tampa General Hospital | Appt: Appointment | NICU: Neonatal Intensive Care Unit | WIC: Supplemental Nutrition Program for Women, Infants, and Children
TGH: Tampa General Hospital | Appt: Appointment | NICU: Neonatal Intensive Care Unit | WIC: Supplemental Nutrition Program for Women, Infants, and ChildrenNetwork map showing agency linkages for referral services