Neonatal Fetal Nutrition & Metabolism 3
Session: Neonatal Fetal Nutrition & Metabolism 3
628 - Effect of Postnatal Steroids on Lean Body Mass in Very Low Birth Weight Preterm Infants
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 628.4638
PRABHU S. PARIMI, Metro Health Medical Center, Clevelabd, OH, United States; Stephanie Merlino Barr, MetroHealth Medical Center, Cleveland, OH, United States; Kelcie O'Dell, MetroHealth, Parma Heights, OH, United States; Luke A. Przybys, MetroHealth Medical Center, Olmsted Falls, OH, United States

Luke A. Przybys
Pre-Medicine Student and Chester Scholar Researcher
Ohio Wesleyan University | MetroHealth Medical Center
Cleveland, Ohio, United States
Presenting Author(s)
Background: Bronchopulmonary dysplasia (BPD) is a major complication in very low birth weight (VLBW) infants and is associated with long-term neurodevelopmental, respiratory morbidity and growth failure. Postnatal corticosteroids (PCS) are frequently used in VLBW infants to interrupt inflammatory cascade and to modify the severity of BPD. Cumulative evidence suggests PCS improves survival of infants without BPD at 36 weeks and at hospital discharge. Approach using BPD prediction model mitigates adverse effects of PCS and on metabolism and growth. The short-term impact of PCS on lean body mass/fat mass in VLBW infants in the setting of complex neonatal issues is unknown. We hypothesized that PCS use in at-risk BPD infants decreases lean body mass and increases fat mass.
Objective: Examine the effect of PCS on Fat mass/Lean body mass in VLBW infants with Bronchopulmonary Dysplasia.
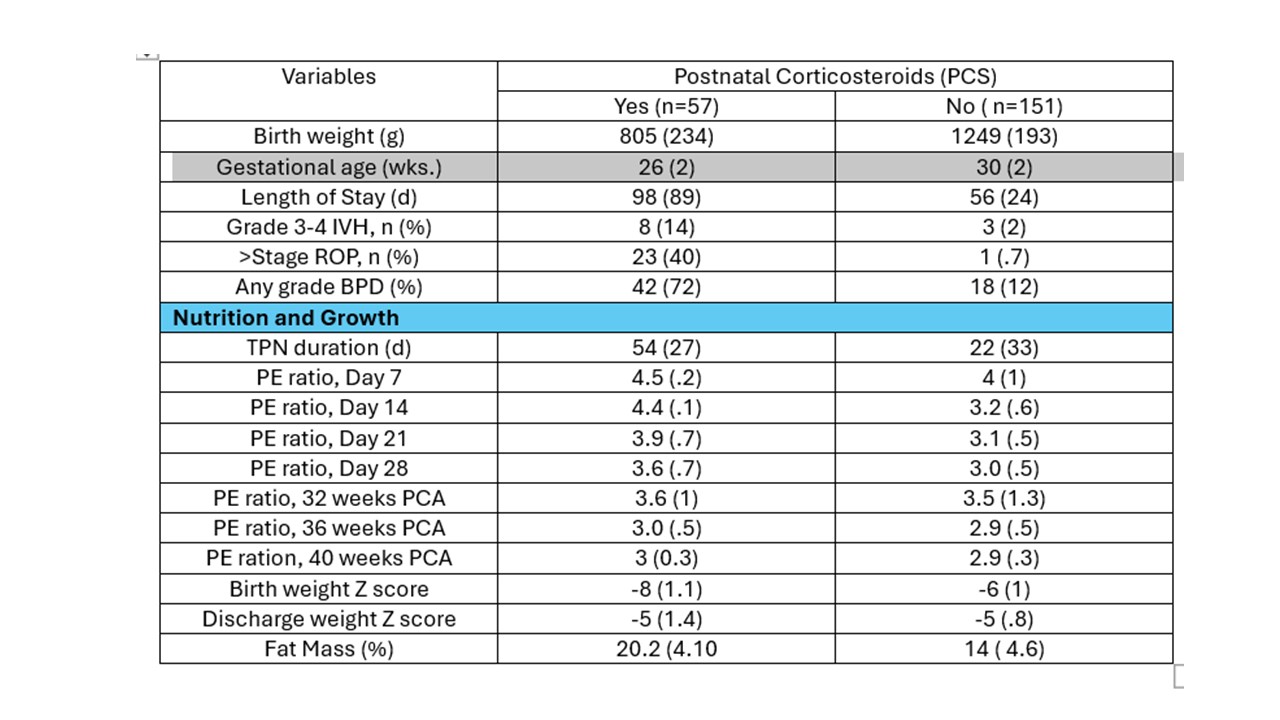
Design/Methods: Infants ≤1500g (n=208) born between 1/2019- 12/2023 were included in this retrospective study. NICHD BPD outcome estimator between 7 to 28 days was used to select infants to initiate PCS (Hydrocortisone or Dexamethasone). Cumulative steroid dose was converted to hydrocortisone equivalence for statistical analysis. Demographic, clinical, neonatal outcome data were collected. Using parenteral and enteral nutrition data, protein to energy ratio (PER) was calculated on 7, 14, 21, 28 days and between 32 to 40 weeks corrected age. Effect of PCS on fat mass and fat-free mass by Air Displacement Plethysmography ( PeaPod ®) was examined, a standard of care in our unit prior to discharge (CA: 36-42 weeks). Univariate analysis and multiple regression models were used to assess the independent effect of PCS on body composition. P<.05 was used for statistical significance.
Results: Among study cohort, 42 (20%) infants met NIH definition of BPD, & among them 57 (27%) met criteria to start PCS. Birth weight, gestational age and neonatal morbidity were significantly different in infants who received PCS. Most importantly, PER was significantly higher between 7-28 days of age in infants receiving PCS (Table 1). Fat mass was significantly higher in PCS group (Figure 1). When controlled for key variables, PCS had no independent effect on Fat mass prior to discharge (Table 2).
Conclusion(s): While gestational age, duration of TPN and PE ratio influenced fat mass, PCS had no independent effect in VLBW infants at risk for BPD. We speculate provision of optimal parenteral and enteral nutritional with a focus on PE ratio provides higher amounts of leucine to counter catabolic effects of PCS as demonstrated by Scott Kimball et al in a preclinical model.
Figure 1. Effect of PCS on Fat Mass
.jpg)
Table 2.
.jpg)
Table 1.
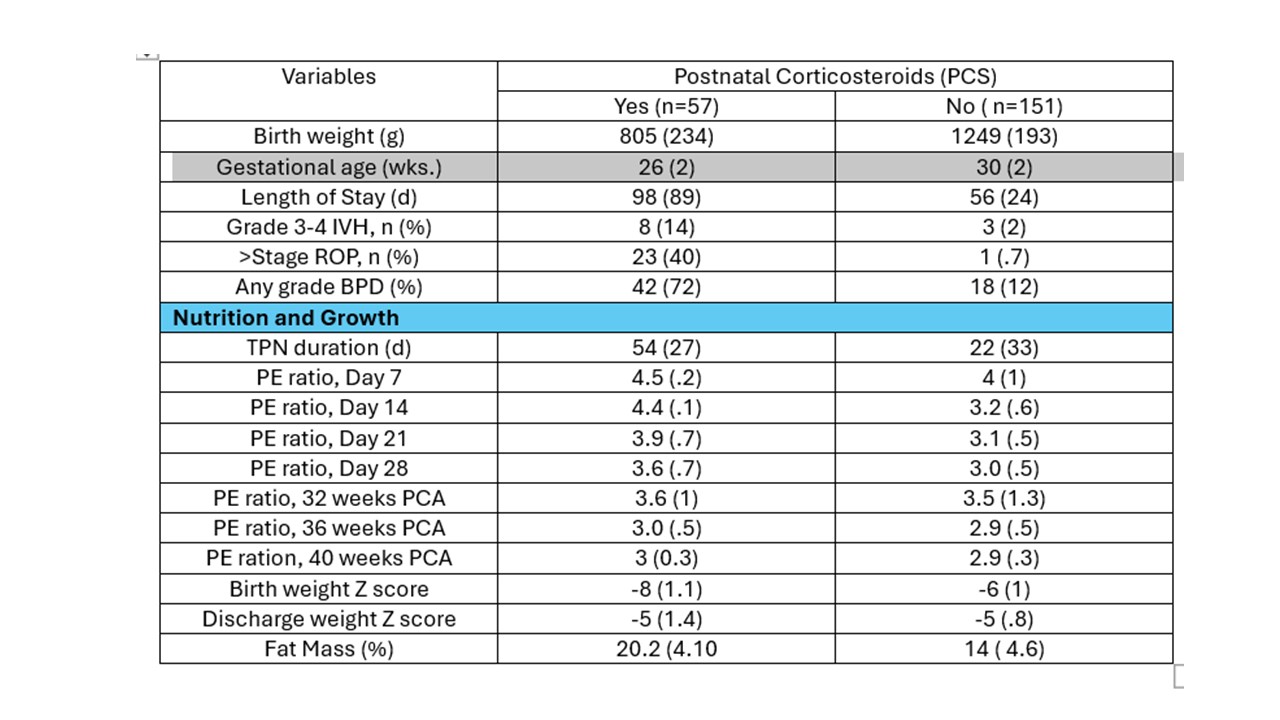
Figure 1. Effect of PCS on Fat Mass
.jpg)
Table 2.
.jpg)
Table 1.