Neonatal General 12: Prenatal Exposures
Session: Neonatal General 12: Prenatal Exposures
431 - Mothers with Concurrent Cocaine and Opioid Use and Neonatal Outcomes
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 431.5924
Divya Rana, UTHSC, Memphis, TN, United States; Massroor Pourcyrous, UTHSC memphis TN, Memphis, TN, United States
- DR
Divya Rana, MD (she/her/hers)
Associate Professor
UTHSC
University of Tennessee Health Science Center
Memphis, Tennessee, United States
Presenting Author(s)
Background: Recently amongst mothers with substance use disorders, there is an emerging trend of using illicit fentanyl with stimulants like cocaine. Cocaine, a stimulant, can enhance euphoria and increase energy levels, while fentanyl, an opioid, provides pain relief and induces sedation. Unfortunately, some individuals misuse these substances concurrently to manipulate their psychoactive effects, seeking to balance the stimulating effects of cocaine with the sedative effects of fentanyl. This practice may heighten the risk of adverse outcomes.
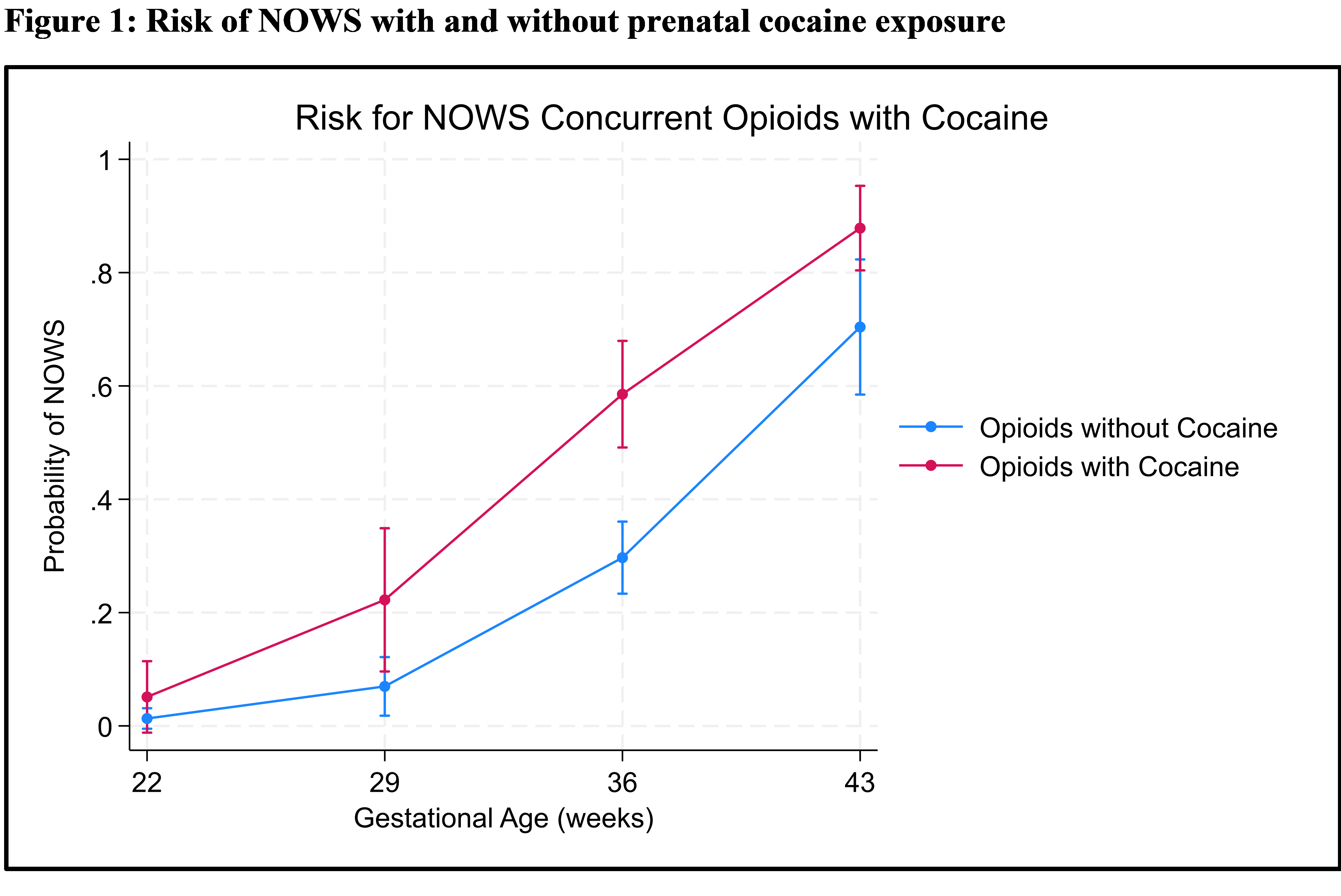
Objective: We wanted to test the hypothesis that neonatal opioid withdrawal syndrome (NOWS) risk decreases with concomitant cocaine and opioid exposure.
Design/Methods: A Prospective observational study of maternal substance use. Data is presented from a cohort born between 2018 through 2022. Maternal substance use was confirmed through screening questionnaire, urine toxicology screening and confirmatory testing with umbilical cord tissue toxicology. Maternal and infant relevant demographic and clinical data was collected. A univariate analysis and regression was used.
Results: A total of 353 infants were born to 342 mothers, with 31% (110/353) of the infants born to women who used cocaine along with opioids. Maternal demographics were comparable; however, significantly fewer women in the cocaine group reported adequate prenatal care, a history of chronic pain, or enrollment in medication for opioid use disorder (MOUD) (p = 0.03). Polysubstance use was prevalent, with a significantly higher incidence of fentanyl and marijuana use in the cocaine group (p < 0.01), Table 1. Infants from both groups had similar mean gestational ages, though there was a trend towards lower birth weights in the cocaine group (p = 0.09). A higher proportion of infants in the cocaine group required treatment for neonatal opioid withdrawal syndrome (NOWS) (p < 0.01) and experienced significantly longer hospital stays (p < 0.01), table 2. Logistic regression analysis indicated that infants diagnosed with NOWS had an average length of stay (LOS) extended by 24 days (p < 0.001). In contrast, preterm infants with NOWS had a non-significant decrease in LOS of 5 days (p = 0.14). Maternal cocaine use did not have a significant effect on LOS (p = 0.11). Regression analysis revealed that maternal cocaine use significantly increased the odds of having NOWS by nearly 6.5 times (p < 0.001), figure 1.
Conclusion(s): Contrary to our hypothesis, our study highlights the significant impact of maternal cocaine use on the increased likelihood of NOWS and extended hospital stays for affected infants.
Table 1. Maternal Demographics
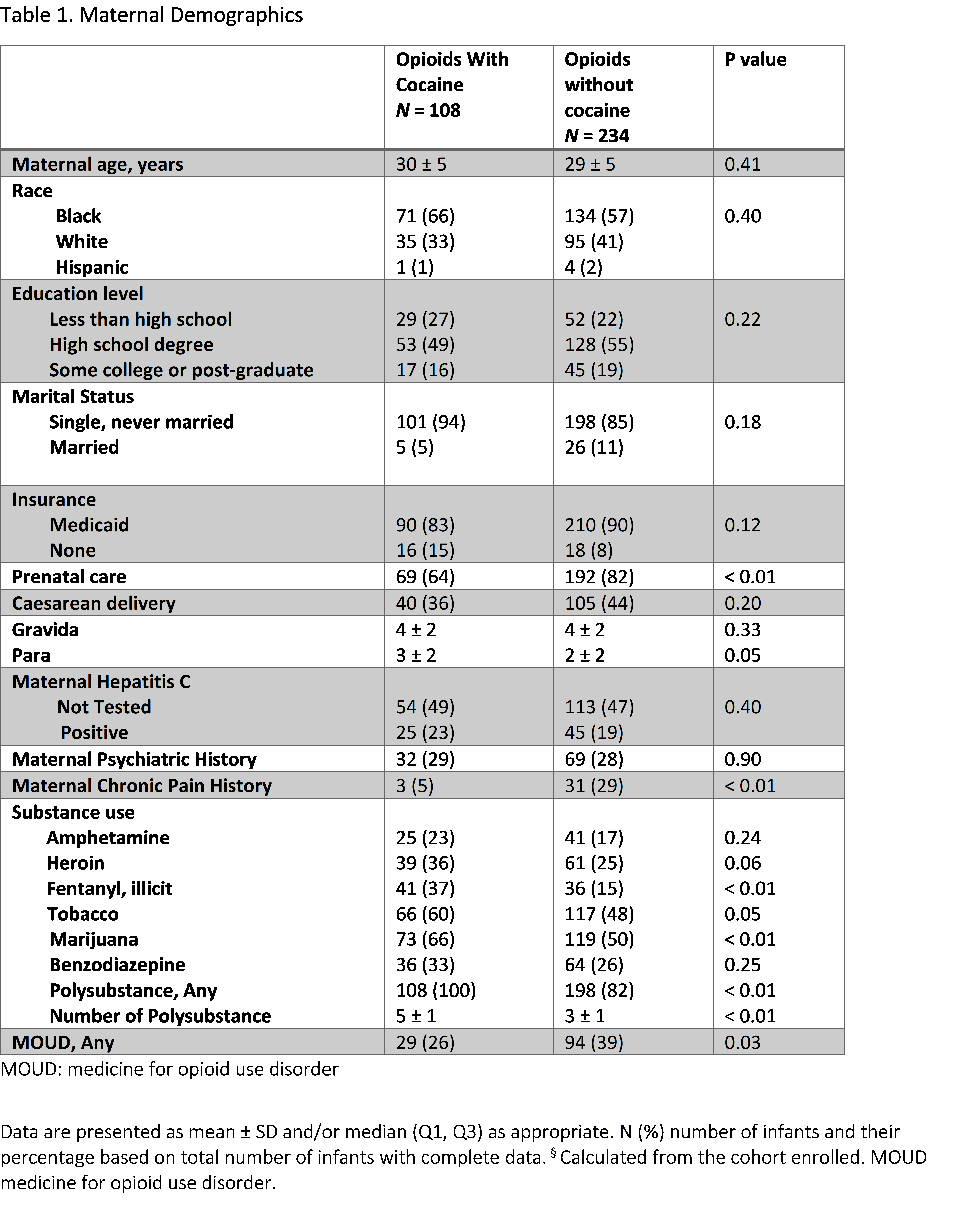
Table 2. Infant Demographics and Outcomes
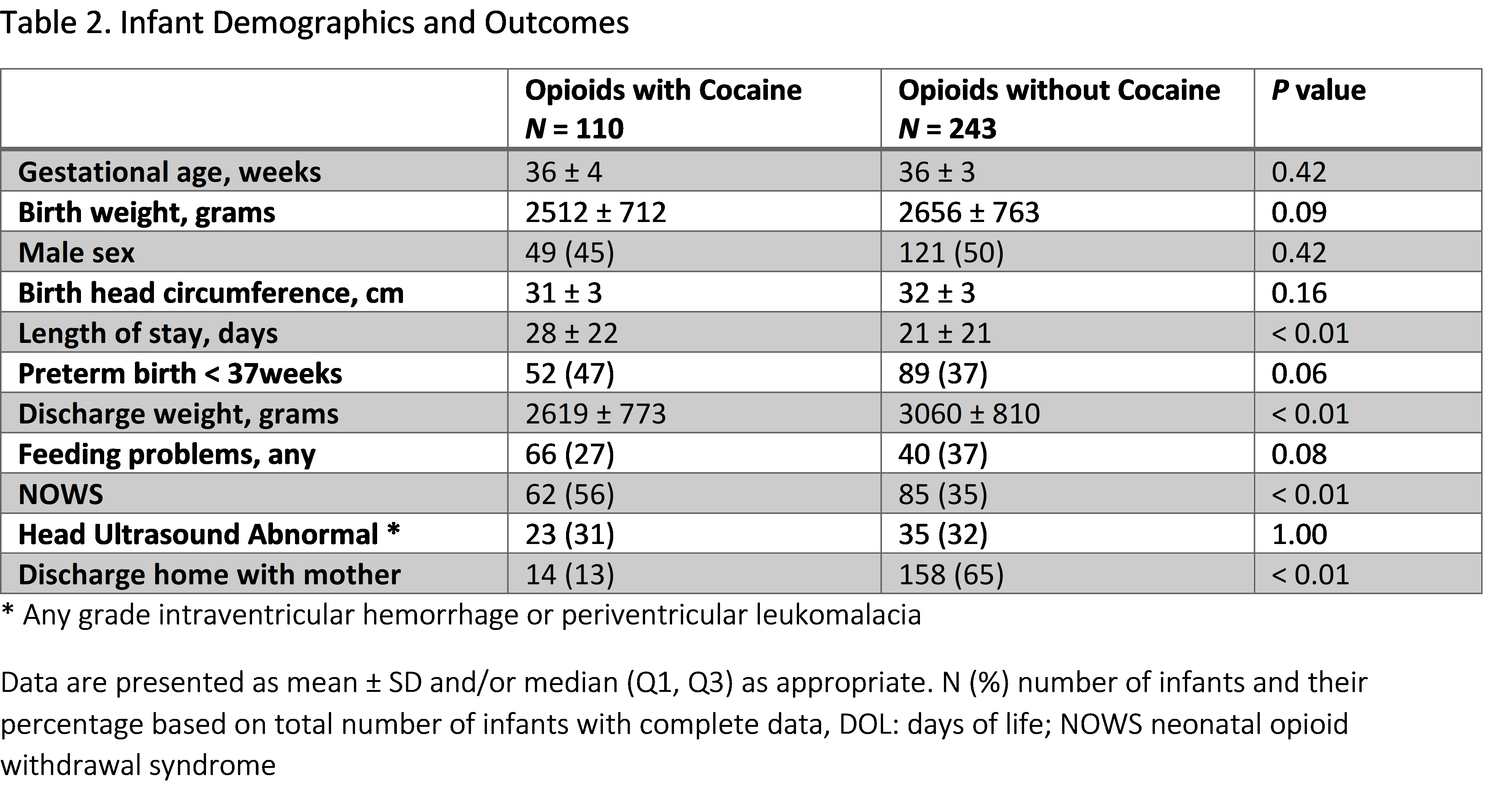
Figure 1: Risk of NOWS with and without prenatal cocaine exposure