Neonatal/Infant Resuscitation 3
Session: Neonatal/Infant Resuscitation 3
385 - Human Factor Considerations for Assisted Ventilation during Delayed Cord Clamping for Extremely Preterm Infants: A Qualitative Study from the VentFirst Trial
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 385.5424
Justin Josephsen, Saint Louis University School of Medicine, Saint Louis, MO, United States; Brenda H. Law, University of Alberta Faculty of Medicine and Dentistry, Edmonton, AB, Canada; Elizabeth Miller, Saint Louis University School of Medicine, St. Louis, MO, United States; Karen Fairchild, University of Virginia School of Medicine, Charlottesville, VA, United States
- JJ
Justin Josephsen, MD
Associate Professor of Pediatrics
Saint Louis University School of Medicine
Saint Louis, Missouri, United States
Presenting Author(s)
Background: Assisted ventilation during delayed cord clamping (AV-DCC) by providing mask ventilation to a newborn infant with the umbilical cord still attached was evaluated as a part of the VentFirst randomized trial. Infants born at 23 0/7 - 28 6/7 weeks were enrolled from 12 study sites across Canada and the US. Providing AV-DCC without interfering with obstetrical management requires thoughtful preparation, training, teamwork, and communication between obstetrical and neonatal teams. In this trial, sites configured teams and equipment to fit their local needs. This pragmatic approach resulted in a rich, multi-centered experience of practicalities and human factors of implementing AV-DCC. Although this intervention has not yet been shown to confer benefit, understanding implementation and barriers is needed to inform future research.
Objective: To describe experience of healthcare providers and researchers in the planning and implementation of the VentFirst intervention. To elicit barriers and facilitators for implementing AV-DCC.
Design/Methods: Research coordinators, neonatologists, neonatal nurses, nurse practitioners, and obstetricians from VentFirst sites participated in semi-structured interviews to describe their experience preparing for and participating in AV-DCC. Interviews were transcribed for thematic analysis.
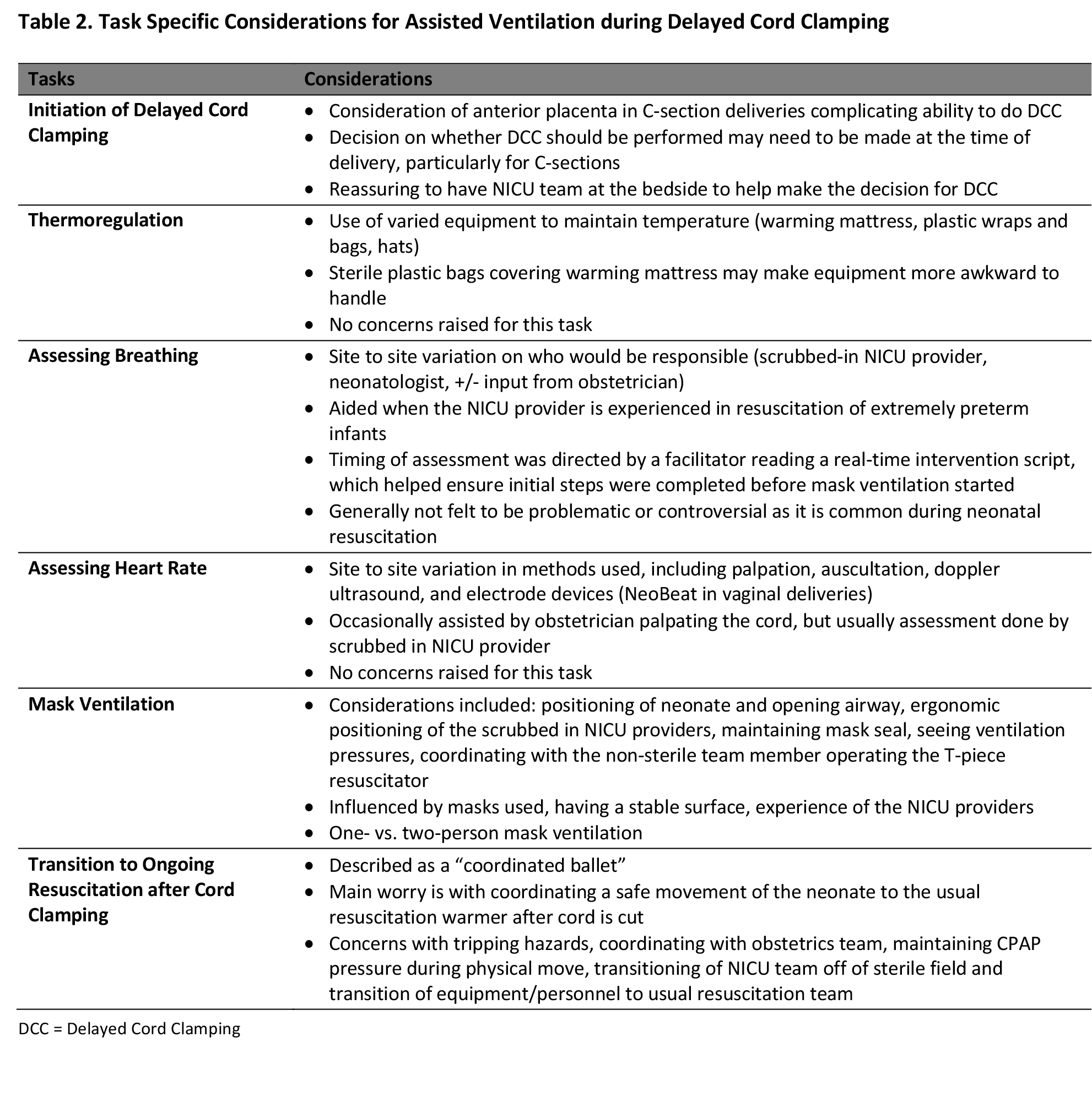
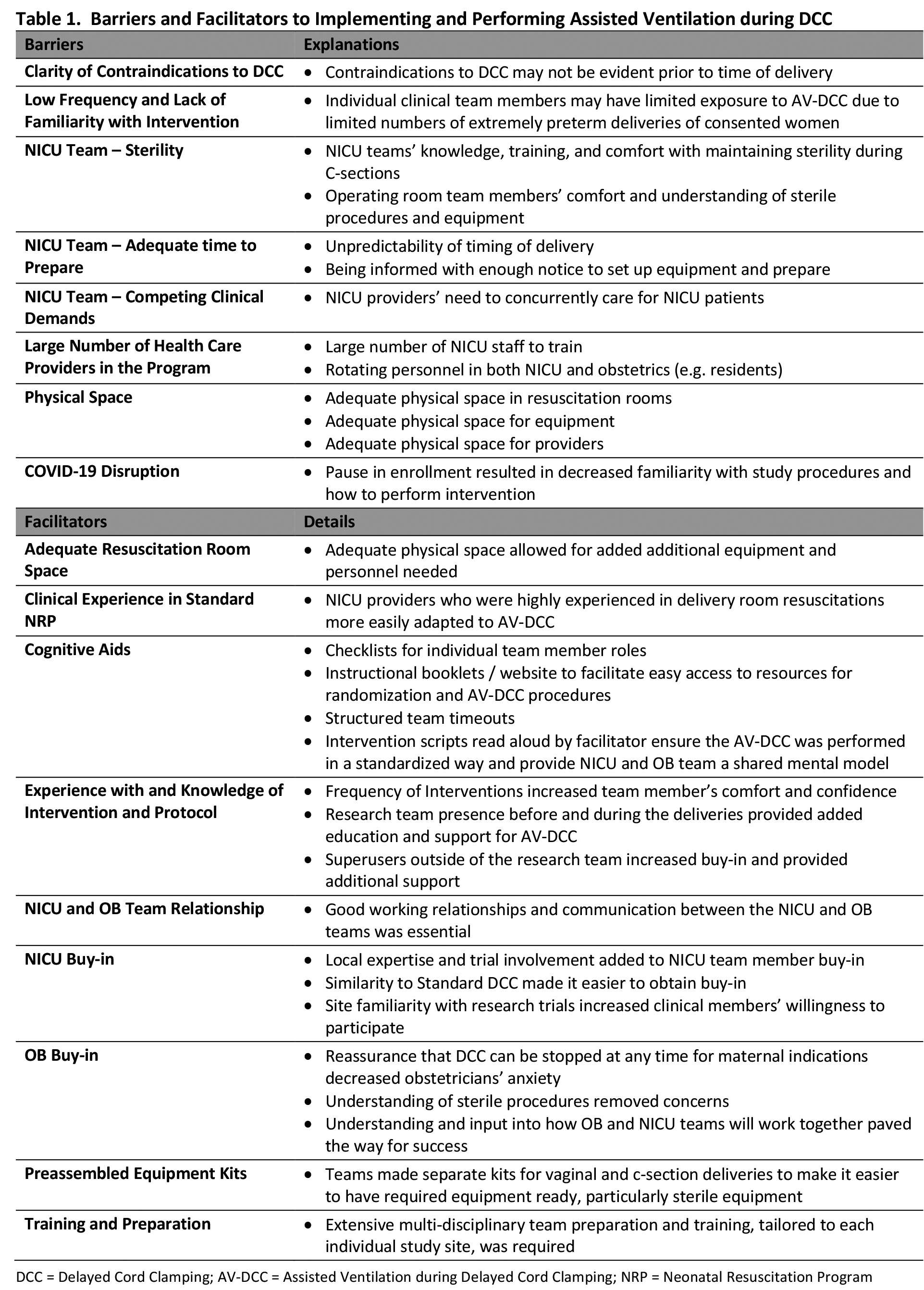
Results: Ten participants from 6 sites were interviewed. Barriers to AV-DCC included: inadequate time to prepare, lack of familiarity with the intervention, physical space issues, and others. Facilitators included: team buy-in, familiarity and practice, training and preparation, cognitive aids, physical space, and clinical experience.(Table 1) Major themes identified include: Equipment Specifics and Considerations, Physical Space, Teamwork and Organizational, Training, Parental Perspectives, Research Process, Applying Learnings to Standard NRP, Future Considerations, and Twin Deliveries.(Figure 1) Participants highlighted key adaptions and challenges to provide thermoregulation, assess breathing, determine heart rate, provide mask ventilation, and transition to post cord clamping care.(Table 2)
Conclusion(s): The potential benefits of AV-DCC remains a subject of research. Successful implementation of AV-DCC depends on careful planning and consideration for equipment, physical space, training, and teamwork. It is facilitated by obstetrical and neonatal collaboration, cognitive aids, and diverse training modalities. Additional interviews are underway to further explore these themes, focusing on both the neonatology and the obstetrical teams’ perspectives.
Barriers and Facilitators to Implementing and Performing Assisted Ventilation during DCC
Themes and Subthemes of Providing Assisted Ventilation during Delayed Cord Clamping
.png)
Task Specific Considerations for Assisted Ventilation during Delayed Cord Clamping