Children with Chronic Conditions
Session: Children with Chronic Conditions 2
505 - “There’s no break!”: Co-designing a parent-to-parent respite navigation intervention to augment respite access for parents of children with medical complexity
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 505.3994
Amy S. Porter, Massachusetts General Hospital, Harvard Medical School, Boston, MA, United States; Ariella Wagner, Tufts University School of Medicine, Framingham, MA, United States; Brittany M. Kelly, Massachusetts General Hospital, Billerica, MA, United States; Sarah Thurlow, Massachusetts General Hospital, Revere, MA, United States; Elizabeth Bostic, MA Department of Public Health, Boston, MA, United States; Sarah J.. Halix, MassGeneral Hospital for Children, Boston, MA, United States; Joanne Wolfe, Massachusetts General Hospital and Brigham and Women's Hospital, Boston, MA, United States; Jennifer Snaman, Dana-Farber Cancer Institute, Boston, MA, United States

Amy S. Porter, MD, PhD (she/her/hers)
Attending Physician
Massachusetts General Hospital, Harvard Medical School
Boston, Massachusetts, United States
Presenting Author(s)
Background: Parents of children with medical complexity (CMC) get few, if any, breaks over decades of intensive caregiving. This unremitting work of care compromises their well-being, their caregiving capacity, and CMC health outcomes, further straining the healthcare system. Respite – short-term direct care – enables parents to take a break, yet few have access to these services.
Objective: This two-phase study first explored CMC parents’ barriers to/facilitators of respite access and then engaged in experience-based co-design (EBCD) to address parents’ respite needs.
Design/Methods: This dual-center study used semi-structured interviews and participant observation with CMC parents and their home-based clinicians to examine parent experiences across 4 domains: work of care, rest, rejuvenation, and respite. Parents or other family caregivers of CMC ≤30 years, living at home, and receiving care from pediatric palliative care/complex care at two academic centers were eligible. Rapid qualitative analysis identified emergent themes. A Community Partner Committee including CMC parents, home-based clinicians, pediatric complex care/palliative care experts, and state Department of Public Health representatives then engaged in EBCD.
Results: In phase I, 21 parents of 20 CMC and 8 home-based clinicians participated. We identified 4 key themes: Parents confirmed (1) their incessant work of care and (2) that respite is critical to well-being and caregiving capacity. They (3) identified lack of bandwidth to pursue respite services as the primary barrier to access and (4) reported that they trust other parents over clinicians to help them navigate resources. In phase II, an 18-member Community Partner Committee developed RECHArge, a parent-to-parent navigation intervention prototype targeting improved respite access (Figure 1). Design session work products included intervention structure/logistics (Figure 2), corresponding intervention manual, and navigator training curriculum content outline.
Conclusion(s): CMC parents desperately need respite yet have limited bandwidth to access it. Parents, themselves, are a critical untapped resource for navigating respite opportunities. Parent-to-parent respite navigation – an intervention co-designed with CMC parents – offers a novel approach to improving respite access. Next steps include pilot testing the intervention and exploring implementation barriers/facilitators to plan for a future efficacy trial. This work aims to augment respite access for CMC parents, a critical component of improving clinical outcomes and managing health resource utilization for CMC.
Figure 1. Impact of peer navigation intervention on CMC and parent caregivers
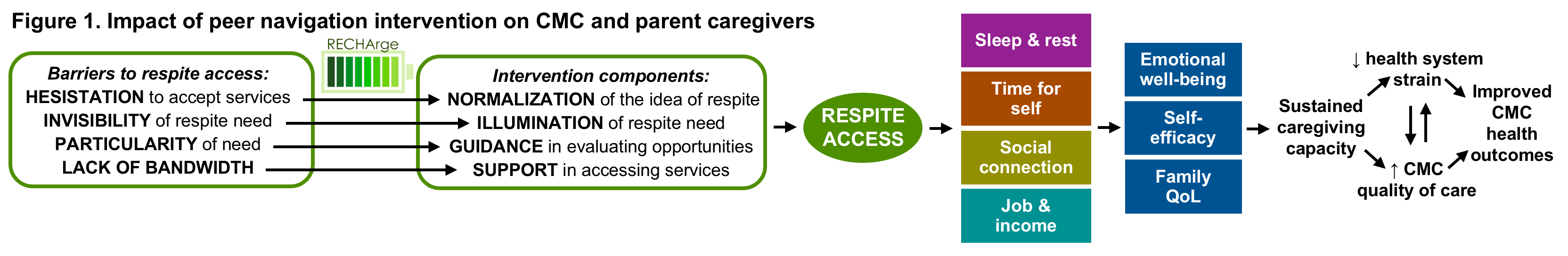
Figure 2. RECHArge intervention
.png)

