Nephrology 5
Session: Nephrology 5
625 - Improving Identification of Acute Kidney Injury (AKI) in Hospitalized Children at HMH K. Hovnanian Children’s Hospital at Jersey Shore University Medical Center
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 625.5565
Eman Hamed, K. Hovnanian Children's Hospital at Jersey Shore University Medical Center, WALL TOWNSHIP, NJ, United States; Guillermo Hidalgo, New Jersey- Hackensack Meridian Health/ K. Hovnanian Children's Hospital, Neptune, NJ, United States; Cathleen Ballance, jersey Shore University Medical Center, Beachwood, NJ, United States; Eman Hamed, JSUMC, Wall, NJ, United States

Daniel Rosenfeld, MD
Resident
K. Hovnanian Children’s Hospital at Jersey Shore University Medical Center
Asbury Park, New Jersey, United States
Presenting Author(s)
Background: Acute Kidney Injury (AKI) is a significant concern in hospitalized pediatric patients but remains underrecognized on the general pediatric floor at JSUMC, where the screening rate is currently 0%. This results in missed diagnoses, delayed interventions, and insufficient data to guide AKI prevention and chronic kidney disease (CKD) risk stratification. Early AKI detection is crucial for improving patient outcomes and reducing long-term renal complications.
Objective: 1. Increase AKI Screening: Raise the screening rate from 0% to 100% by April 2025.
2. Enhance Awareness: Improve resident and hospitalist knowledge on AKI risk factors, diagnostic criteria, and the importance of screening.
3. Standardize Risk Factor Identification: Ensure consistent identification of AKI risk factors, such as nephrotoxic medications, previous AKI, CKD, sepsis, and prematurity.
4. Standardize Screening Tools: Develop and implement tools to facilitate consistent AKI screening and early detection.
Design/Methods: 1. Education and Awareness
o Grand Rounds: Deliver educational sessions on AKI risk factors and detection strategies to residents and hospitalists.
o Laminated Cards: Distribute cards outlining AKI risk factors and normal creatinine values for quick reference.
2. Integration into Daily Clinical Practice
o IPASS Tool Integration: Add an AKI screening tool to the resident H&P template and IPASS handoff sheet to prompt risk factor screening.
o Documentation & Tracking: Use MRNs to track screening rates, document findings, and ensure AKI is added to the problem list when applicable.
o Team-Led Screening: Assign a team leader each week to ensure AKI screening and documentation.
3. Feedback and Continuous Improvement
o PDSA Cycles: Use the Plan-Do-Study-Act methodology to refine strategies and review data to improve screening and documentation.
Results: • PDSA Cycle 1: Screening rate increased from 0% to 50%, and AKI diagnoses increased to 7.6%.
• PDSA Cycle 2: Screening rate reached 56%, with 22% of patients diagnosed with AKI.
• PDSA Cycle 3: Screening rate increased to 94%, with 25% of patients having AKI documented.
Conclusion(s): The study has shown promising results in improving AKI screening rates, detection of risk factors, and diagnoses. This indicates that the tools and strategies; AKI toolbox IPASS integration, laminated cards, and education sessions, are effective in prompting AKI screenings. However, the percentage of patients diagnosed with AKI, having AKI added to their problem list and Nephrology follow-ups scheduled remains lower than expected, suggesting that refinement of the screening process is necessary.
CV_PERMIT.pdf
Figure 2: PDSA Cycle 2 Using Laminated Cards for Creatinine Normal Values
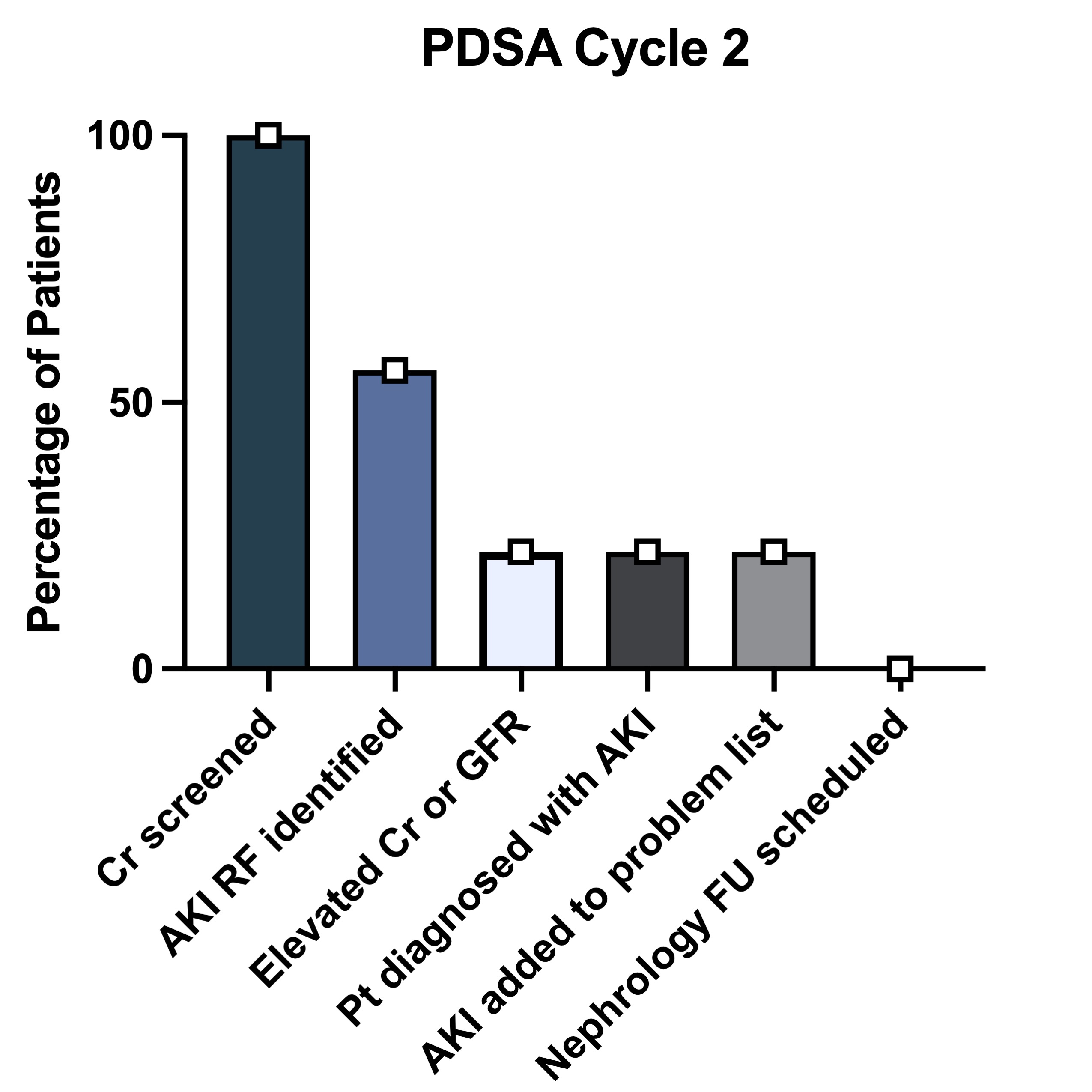 o AKI Screening Rate: Increased to 56%.
o AKI Screening Rate: Increased to 56%.o Detection of Risk Factors: Increased to 100%.
o AKI Diagnosis Rate: 22% of hospitalized patients diagnosed with AKI, added to the problem list.
o 0% Nephrology follow-ups scheduled
Figure 3: PDSA Cycle 3 Using Electronic MRN-based Data Collection for Improved Documentation
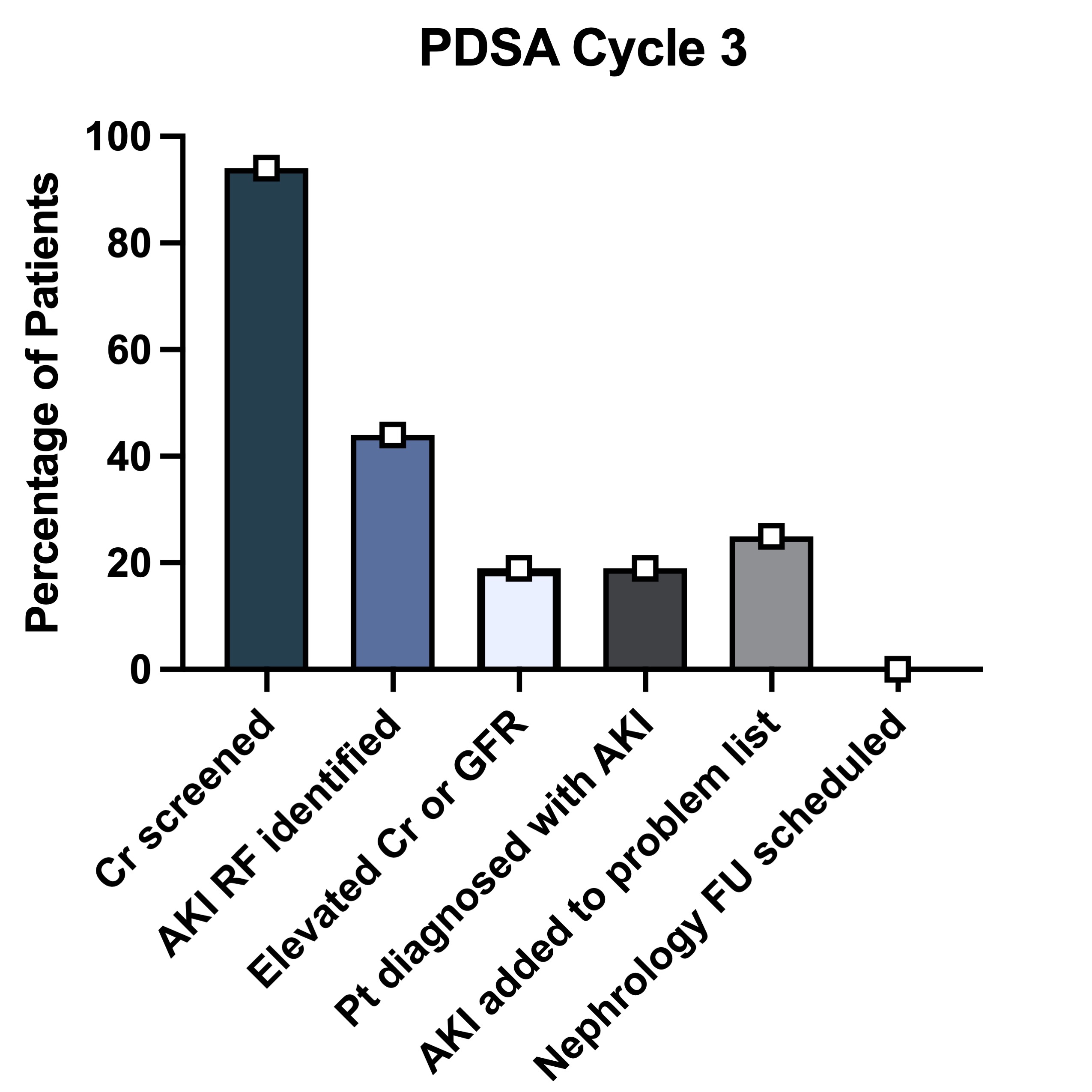 o AKI Screening Rate: Increased to 94%.
o AKI Screening Rate: Increased to 94%.o Detection of Risk Factors: Increased to 44%.
o AKI Diagnosis Rate: 19% of hospitalized patients diagnosed with AKI.
o AKI Documentation Rate: 25% of hospitalized patients had AKI added to their problem list.
o 0% Nephrology follow-ups scheduled


