General Pediatrics 2
Session: General Pediatrics 2
720 - Variability in the Diagnosis of Pediatric Acute Concussion in Massachusetts: A Survey Study
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 720.7053
Prarthana Pilla, University of Massachusetts Medical School, Houston, TX, United States; Sage A. Herbert, Boston University School of Public Health, Brookline, MA, United States; Katie Gu, University of Massachusetts Medical School, Rohnert Park, CA, United States; Theodore Macnow, UMass Memorial Children's Medical Center, Wayland, MA, United States; Arvin Garg, UMass Memorial Children's Medical Center, Worcester, MA, United States; Erin Meyer, UMass Memorial Children's Medical Center, Natick, MA, United States

Prarthana Pilla, BS, MSSP (she/her/hers)
Research Coordinator II
University of Massachusetts Medical School
Houston, Texas, United States
Presenting Author(s)
Background: Pediatric concussion is a growing national and local health problem, typically managed in primary care settings but also in the emergency department. Few studies have examined how the diagnosis of acute pediatric concussion differs by clinician specialty.
Objective: To describe patterns and variability in diagnosis of pediatric acute concussion among primary care and emergency medicine clinicians.
Design/Methods: We conducted a cross-sectional survey study among general pediatric (GP), family medicine (FM), pediatric emergency medicine (PEM), and emergency medicine (EM) clinicians in central Massachusetts who manage acute ( < 72 hours after injury) concussion in children ages 5 to 17 years. We assessed clinician experience with pediatric concussion and practice patterns around the diagnosis of pediatric concussion. We collected data on clinician demographics, clinical training, and practice settings. Descriptive statistics summarized clinician responses and diagnostic practices, stratified by clinician type. We used Fisher’s exact test to detect significant differences by clinician type.
Results: Eighty-three clinicians completed the survey, accounting for 43% of invited clinicians (Table 1). 99% of respondents reported having ever diagnosed a pediatric acute concussion, 90% within the past 6 months, and all reported that the majority ( < 50%) of children they diagnose with concussion present within the first 72 hours. Likert scale responses are presented in Figure 1. EM clinicians reported feeling less confident in their ability to recognize signs and symptoms compared to other specialties. GP and FM clinicians inquired about risk factors for prolonged recovery more often than other specialties. FM and GP were significantly less likely to evaluate cervical spine range of motion and tenderness compared to EM and PEM. GPs (76%) and FM (83%) clinicians were significantly more likely than PEM (30%) and EM (20%) clinicians to have reported ever using a standardized symptoms scale or assessment to aid with acute concussion diagnosis. Only one clinician reported ever using a standardized visio-vestibular assessment to support diagnosis.
Conclusion(s): Most clinicians are confident in their ability to recognize pediatric concussion and felt that it was their responsibility to do so. Nevertheless, there are significant differences in diagnostic practices, specifically the evaluation of risk factors for prolonged recovery, cervical spine assessments, and the use of standardized symptom scales. This work will help inform future efforts to standardize pediatric concussion care across specialties.
Table 1. Demographic and clinical practice characteristics of survey respondents.
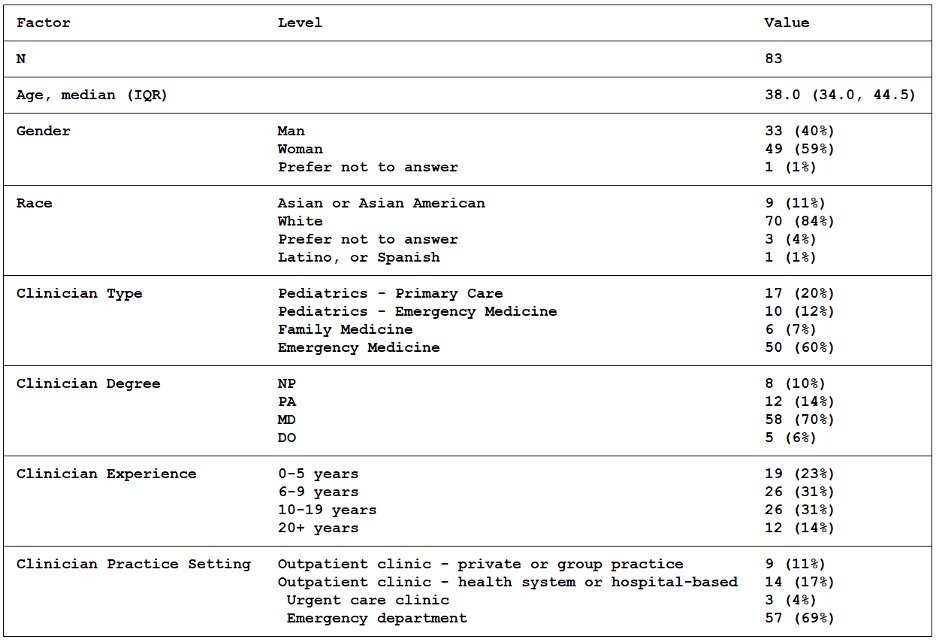
Figure 1. Likert scale responses stratified by clinician specialty
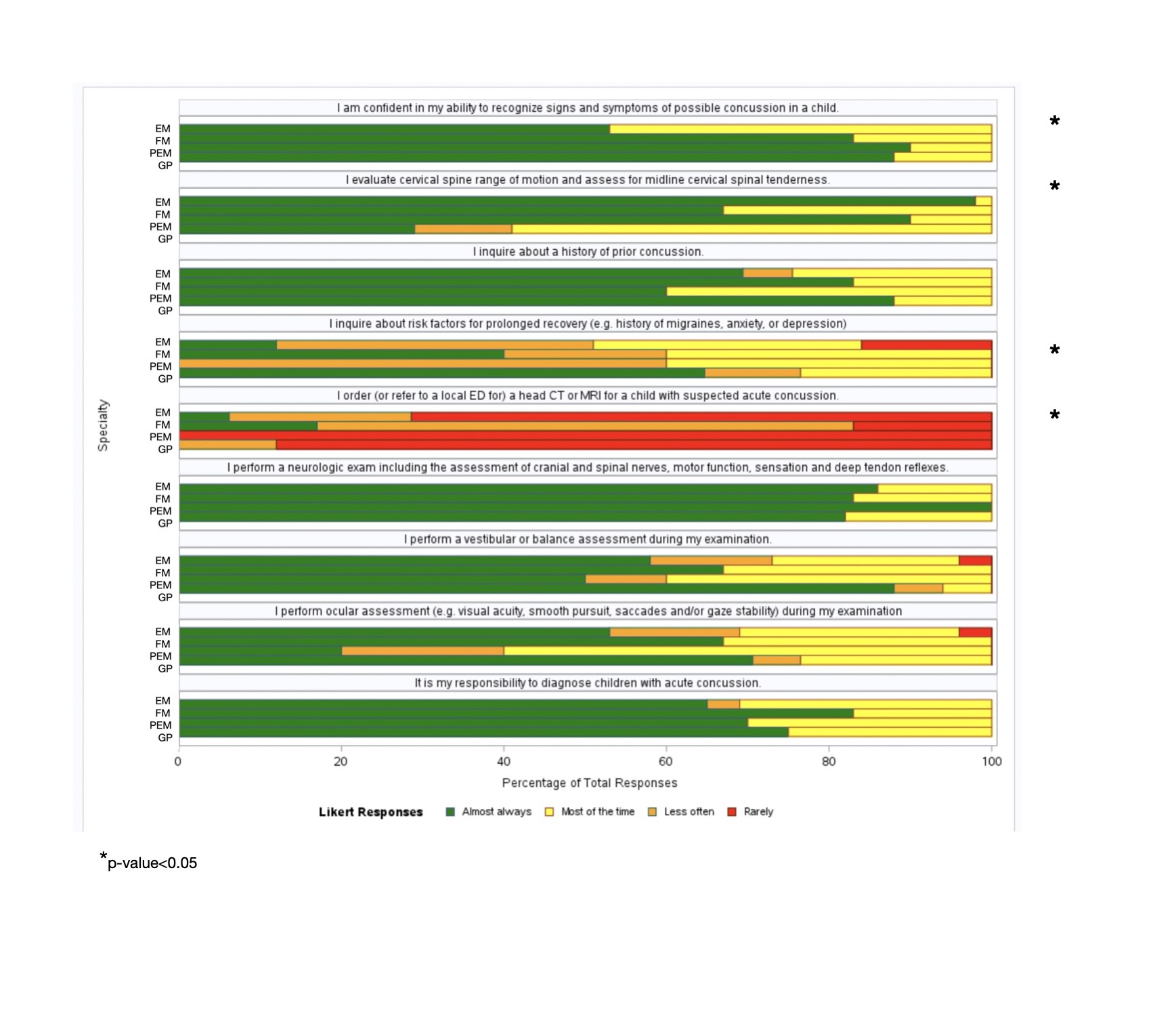 GP = general pediatric, FM = family medicine, PEM = pediatric emergency medicine, EM = emergency medicine.
GP = general pediatric, FM = family medicine, PEM = pediatric emergency medicine, EM = emergency medicine.*Significant differences detected across groups (p < 0.05)

