Emergency Medicine 3
Session: Emergency Medicine 3
449 - Variation in management of hypothermic infants presenting to the emergency department
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 449.7003
Nathan Money, University of Utah School of Medicine, Salt Lake City, UT, United States; Sriram Ramgopal, Ann & Robert H. Lurie Children's Hospital of Chicago, Oak Park, IL, United States; Paria M. Wilson, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Wendi Wendt, Medical College of Wisconsin, Milwaukee, WI, United States; Andrea T. Cruz, Baylor College of Medicine, Houston, TX, United States; Sofia Grigoria Athanasopoulou, Yale School of Medicine, New Haven, CT, United States; Jamie Holland, Medical College of Wisconsin, Milwaukee, WI, United States; Naghma S. Khan, Emory University School of Medicine, ATLANTA, GA, United States; Leslie Ann. Hueschen, Children's Mercy Hospital/ University of Missouri-Kansas City, Kansas City, MO, United States; Paul L. Aronson, Yale School of Medicine, New Haven, CT, United States; Amy D. Thompson, Nemours Children's Hospital, Wilmington, DE, United States; Oluwakemi Badaki-Makun, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Kelly R.. Bergmann, Children’s Minnesota, University of Minnesota Masonic Children’s Hospital, Minneapolis, MN, United States; Laura F. Sartori, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Stacey L. Ulrich, Rady Children's Hospital San Diego, san diego, CA, United States; Theodore Heyming, CHOC Children's Hospital of Orange County, Orange, CA, United States; Amy Zhou, University of Texas Southwestern Medical School, Dallas, TX, United States; Alexandra Geanacopoulos, Boston Children's Hospital, Boston, MA, United States; Alexander Rogers, University of Michigan Medical School, Ann Arbor, MI, United States

Nathan Money, DO (he/him/his)
Assistant professor
University of Utah
Lehi, Utah, United States
Presenting Author(s)
Background: Infants with hypothermia are at risk of occult infections. No evidence-based guidelines exist to guide management of these infants, and prior studies describing variations in care in this population have been limited by sample size.
Objective: Evaluate variation in the management of hypothermic infants presenting to pediatric emergency departments (EDs) in a nationally representative cohort.
Design/Methods: Retrospective cohort study of infants ≤90 days with a rectal temperature of < 36.5 °C in the ED from January 1, 2013, to December 31, 2022 at 16 sites. Patients arriving in cardiac arrest were excluded. We evaluated variation in diagnostic workup, antimicrobial use, and disposition, stratified by age and by lowest degree of hypothermia.
Results: We included 45,673 infants (median age 25 days [IQR 6-52; 52.9% male). A quarter of infants were < 1 week old (27.7%), and most had temperatures between 36.0-36.4 °C (83.9%, Table 1). There was broad interinstitutional variation in testing for blood culture (12.9%-31.4%), urine studies (6.5%-36%), cerebral spinal fluid (3.9%-27.7%), and herpes simplex virus (1.5%-16.6%, Figure). Admission rates varied from 35.9%-59.2%, while empiric antibiotic rates varied from 3.5%-32.5% and empiric acyclovir from 0.7%-17.2%. A higher proportion of infants 0-7 days had empiric antibiotic therapy (17.9% vs 8.6%), hospitalization (57.2% vs 36.9%), and intensive care unit admission (19.1% vs 10.1%) when compared to the rest of the cohort, despite having shorter length of stay (43 vs 54 hours) and lower mortality 0.1% vs 0.2; p< 0.001 for all comparisons [Table 2]). Infants with temperatures < 35.0 °C had higher rates of empiric antibiotic therapy (55.3% vs 10.0%), hospitalization (86.4% vs 41.4%), intensive care utilization (61.6% vs 11.2%), mortality (3.5% vs 0.1%), and longer length of stay (131 vs 46 hours) when compared to the rest of the cohort (p < 0.001 for all comparisons).
Conclusion(s): Substantial interinstitutional variation exists in the workup and management of hypothermic infants in the ED. Younger infants (≤7 days) more frequently received invasive testing and empiric antimicrobials despite having shorter hospital stays and lower mortality. Infants with lower temperatures had higher utilization and more severe outcomes. Further analysis of risk factors for bacterial infections in hypothermic infants is required to develop evidence-based guidelines and standardize care provided to this population.
Figure
.jpg) Inter-hospital variation among 16 hospitals in the care of hypothermic infants presenting to the emergency department. Median value is represented by the dark horizontal line, interquartile range by the shaded box area, and range by the vertical line.
Inter-hospital variation among 16 hospitals in the care of hypothermic infants presenting to the emergency department. Median value is represented by the dark horizontal line, interquartile range by the shaded box area, and range by the vertical line. Table 1
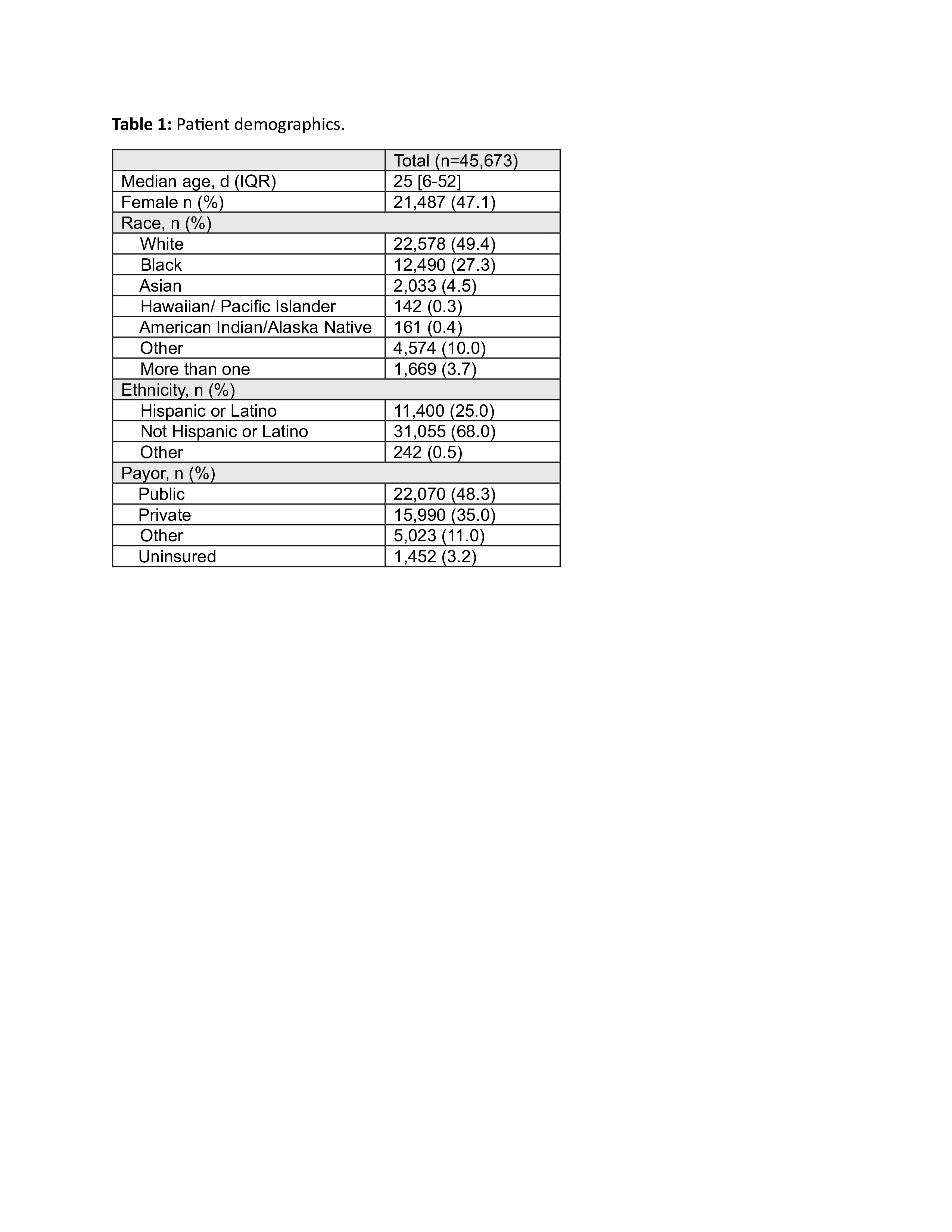 Patient demographics.
Patient demographics.Table 2
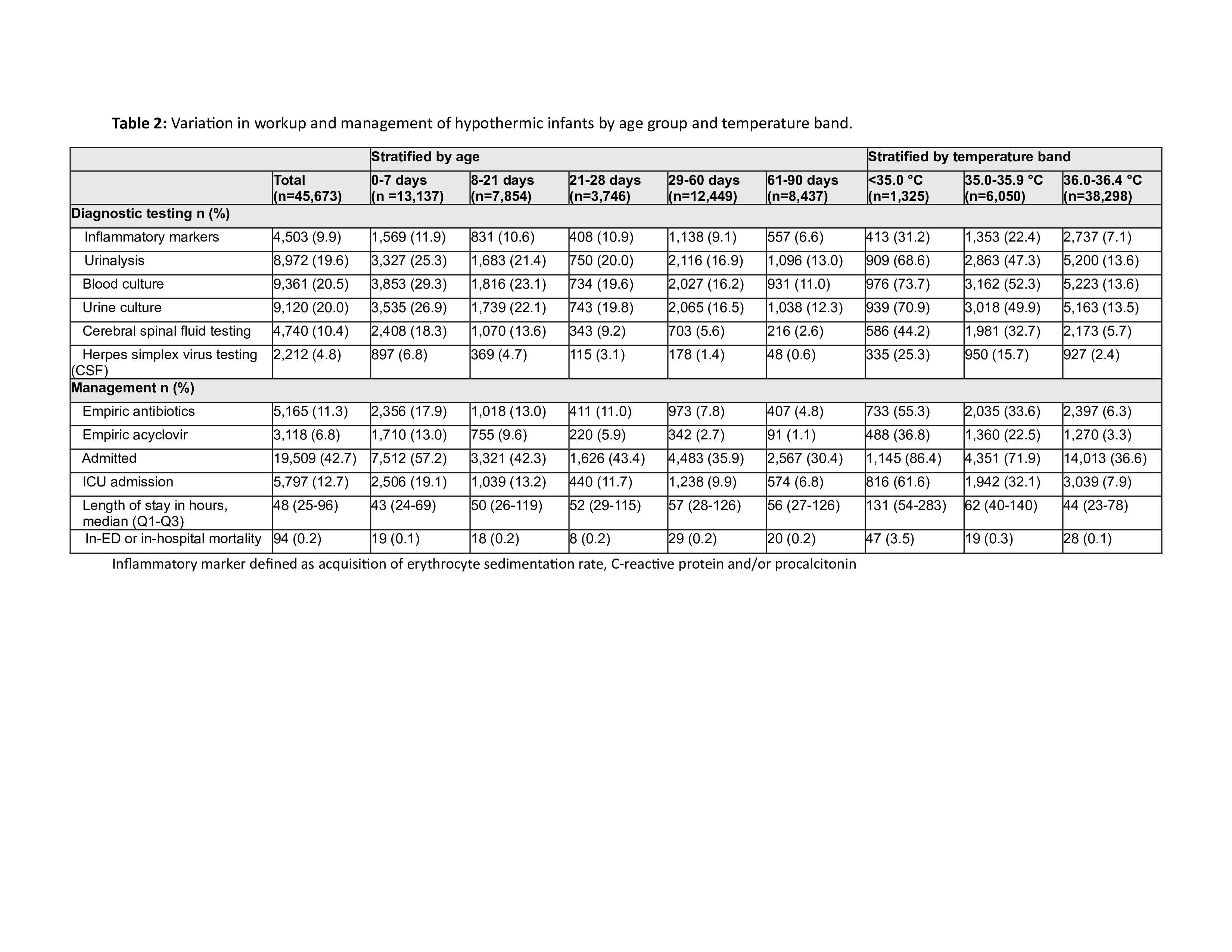 Variation in workup and management of hypothermic infants by age group and temperature band.
Variation in workup and management of hypothermic infants by age group and temperature band. Figure
.jpg) Inter-hospital variation among 16 hospitals in the care of hypothermic infants presenting to the emergency department. Median value is represented by the dark horizontal line, interquartile range by the shaded box area, and range by the vertical line.
Inter-hospital variation among 16 hospitals in the care of hypothermic infants presenting to the emergency department. Median value is represented by the dark horizontal line, interquartile range by the shaded box area, and range by the vertical line. Table 1
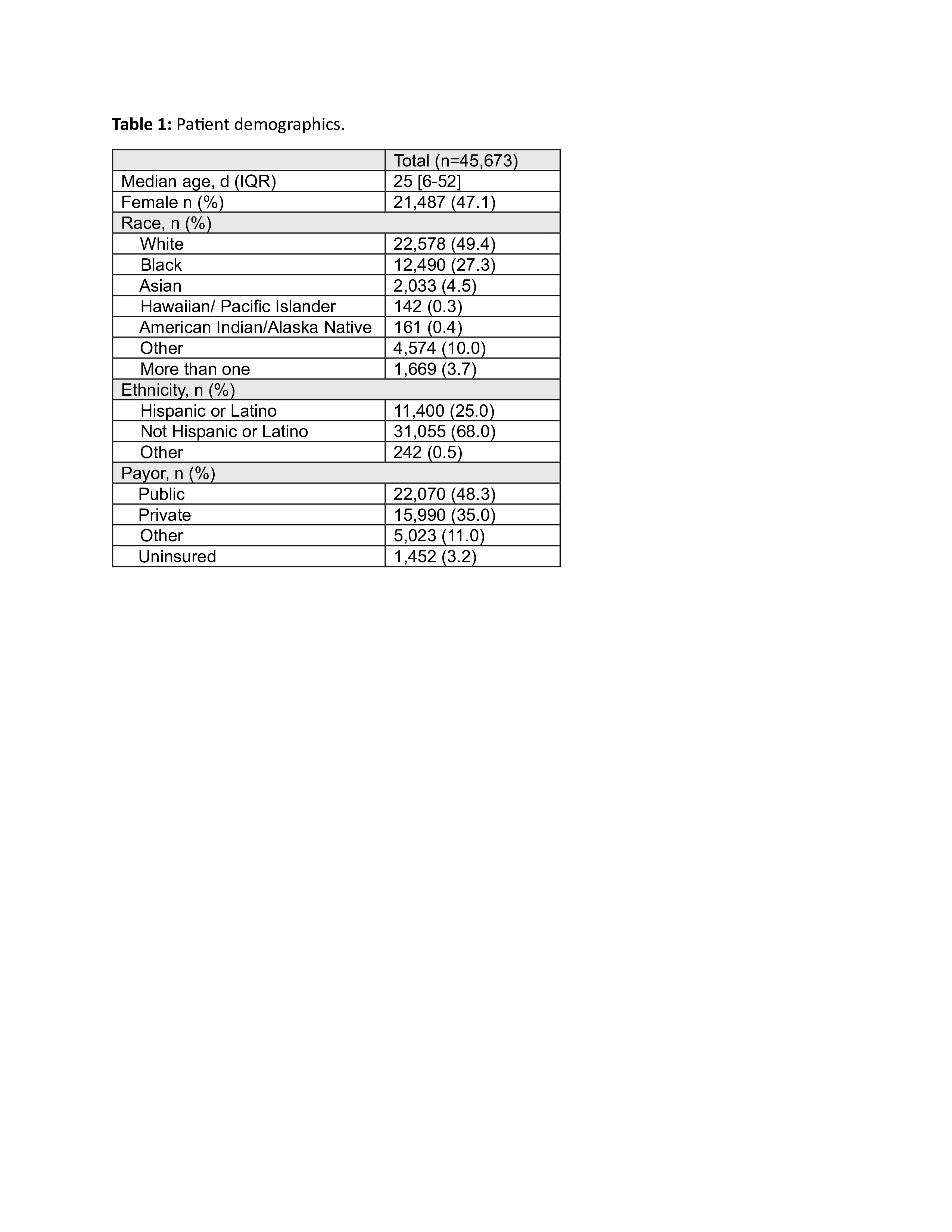 Patient demographics.
Patient demographics.Table 2
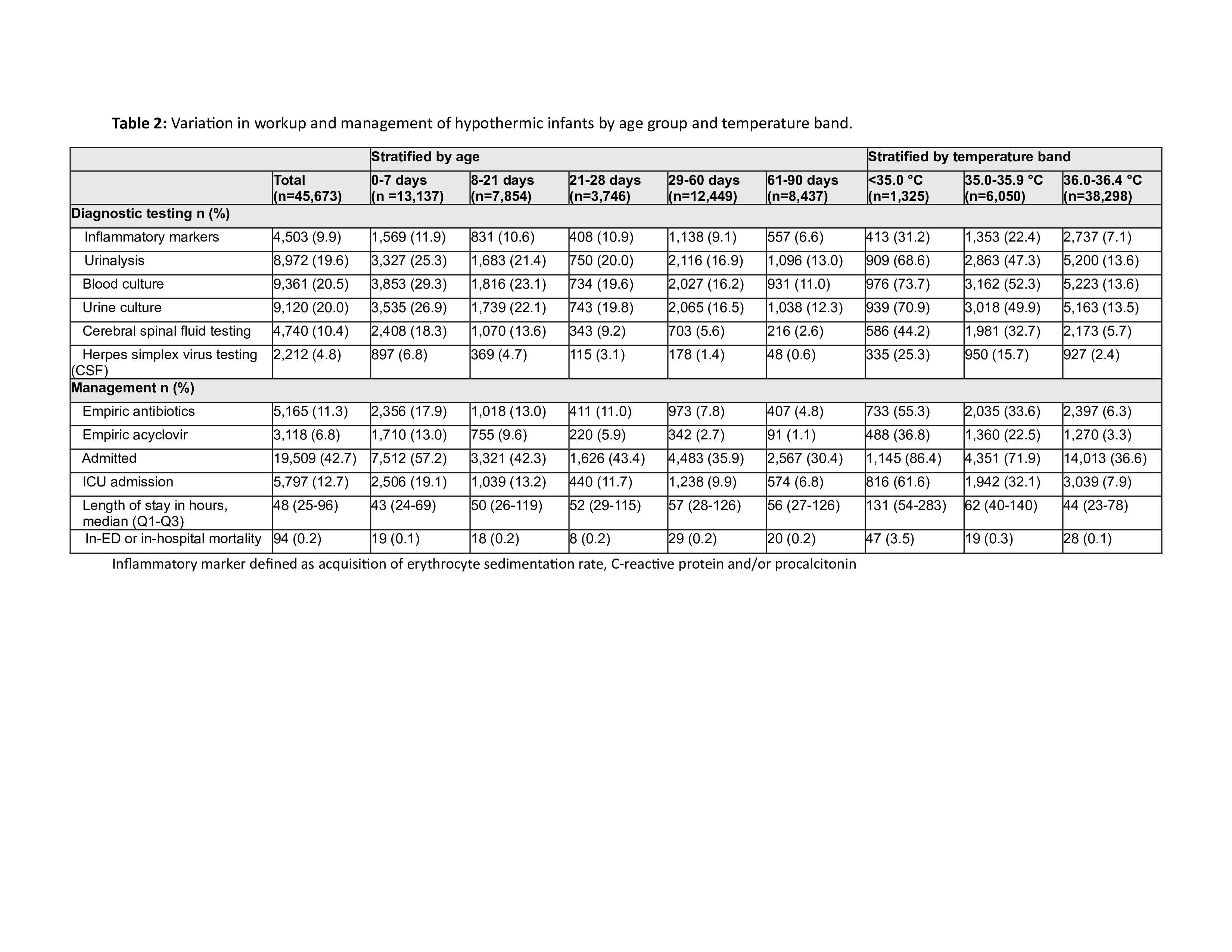 Variation in workup and management of hypothermic infants by age group and temperature band.
Variation in workup and management of hypothermic infants by age group and temperature band. 
