Allergy, Immunology, and Rheumatology 2
Session: Allergy, Immunology, and Rheumatology 2
654 - Successful Incorporation of Resident Subspecialty Education on an Inpatient Hospital Pediatrics Service
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 654.6964
Shauna Schord, Nationwide Children's Hospital, Columbus, OH, United States; Lauren Harper, Loma Linda University Children's Hospital, Redlands, CA, United States; Vinchelle Hardison, Nationwide Children's Hospital, Philadelphia, PA, United States; Christine Bearer, Akron Children's Hospital, Akron, OH, United States; Cara E. Texler, Ohio State University College of Medicine, Columbus, OH, United States; Claire Sevov, Nationwide Children's Hospital, Columbus, OH, United States; Kendra Lauer, Rheumatology, Columbus, OH, United States; Ivana NMN. Stojkic, Nationwide Childrens, Columbus, OH, United States; Samantha Coss, Nationwide Children's Hospital, Columbus, OH, United States; Joanne Drew, Nationwide Children's Hospital, Columbus, Ohio, OH, United States; Jason Benedict, Ohio State University, Columbus, OH, United States; Kyla D. Driest, Nationwide Children's Hospital, Columbus, OH, United States

Kyla D. Driest, MD, MEd (she/her/hers)
Fellowship Program Director
Nationwide Children's Hospital
Columbus, Ohio, United States
Presenting Author(s)
Background: Approximately 300,000 children in the United States have a rheumatologic condition, yet many pediatric residents have limited exposure to Pediatric Rheumatology. To address this knowledge gap – which is a likely contributor to the understaffing of the field – our team of Pediatric Hospitalists and Rheumatologists jointly developed a curriculum that can be delivered within the often hectic inpatient schedule of a general pediatrics team while providing residents with a fundamental knowledge of Rheumatology through asynchronous, case-based learning.
Objective: To improve resident knowledge and confidence in rheumatologic conditions
Design/Methods: We implemented a 4-week case-based Rheumatology curriculum for residents on a general pediatrics hospitalist service. Each week, fellows and faculty presented cases illustrating foundational rheumatologic conditions. Over two 30-minute teaching sessions per week, residents received the case presentation and background followed by management considerations. Teams also received open-ended question-based worksheets each week to facilitate asynchronous team-based learning. One week prior to the rotation, residents received a REDCap survey with demographic information, questions on their attitude toward and prior experiences with Pediatric Rheumatology, and a baseline knowledge quiz covering topics addressed in the curriculum. Survey participation was voluntary. One month after the rotation, participants completed a post-intervention survey that assessed their retention of and confidence in their knowledge of topics covered in the curriculum. Pre- and post-intervention knowledge scores were analyzed using a paired t-test.
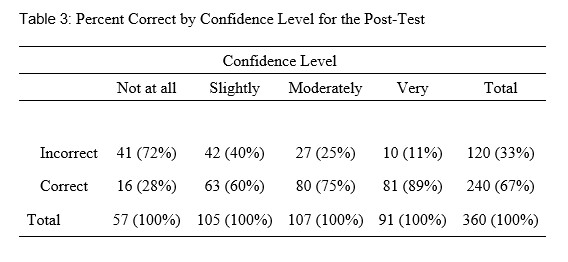
Results: Both surveys were completed by 20/47 eligible participants. There was an average improvement of 12.1% pre- to post-intervention (p < 0.001). Residents were more confident in their answer choices following the intervention with a 96% increase in the number of answers that were marked as “moderately” or “very” confident. Despite the brief nature of the didactics, 70% of the participants “agreed” or “strongly agreed” that they were able to establish rapport with the Rheumatology consult team. Additionally, 50% of participants answered that the field of Rheumatology interested them.
Conclusion(s): Given brief, twice weekly didactics over a 4-week rotation, pediatric residents improved their rheumatologic knowledge and retained it at one month. Further, their confidence in their knowledge improved, they became familiar with the care of patients hospitalized with rheumatologic conditions, and many expressed interest in the field of rheumatology.
Table 1: Demographics of Resident Participants
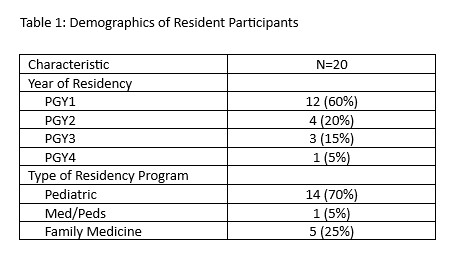
Table 2: Percent Correct by Confidence Level for the Pre-Test
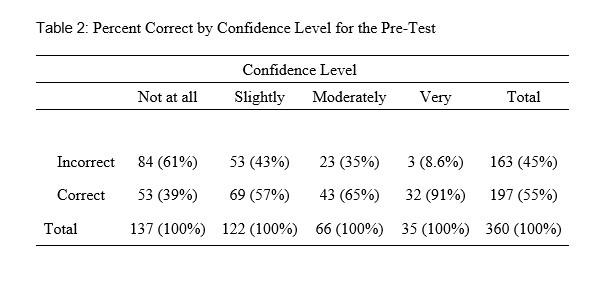
Table 3: Percent Correct by Confidence Level for the Post-Test