Critical Care 2
Session: Critical Care 2
119 - "The Good Doctor": Critical Care Clinician Perspectives on Characteristics of a Good Doctor
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 119.3919
Sarah Jaffar, Children's National Health System, Washington, DC, United States; Amy H. J.. Wolfe, Children's National Health System, Washington DC, DC, United States

Sarah Jaffar, MD (she/her/hers)
Fellow Physician, Pediatric Critical Care
Children's National Health System
Washington, District of Columbia, United States
Presenting Author(s)
Background: The Good Parent literature by Hinds et al described behaviors that caregivers aspire to uphold and the impact of clinicians in support or in conflict with those goals. While behaviors to support the good parent framework were identified, there is a gap in understanding how clinician priorities might be in conflict with caregivers. By defining the good doctor, our hope is to better understand ICU clinician priorities and improve care delivery by aligning with caregivers' goals for their children
Objective: The aim of this study was to describe ICU clinician characteristics of a "good doctor" based on physician and APP perspectives. The secondary aim was to identify barriers which prevent caregiver alignment between the "good doctor" and the previously described "good parent" principles.
Design/Methods: We conducted a prospective qualitative study of pediatric and cardiac ICU physicians and advanced practice providers to describe characteristics of a "good doctor". Additionally, we explored facilitating factors and barriers to clinician achievement of those ideals as well as clinician and family alignment. We applied thematic content analysis to the transcribed semi-structured interviews to create codes, and ultimately themes.
Results: We enrolled 29 clinicians. Clinician themes of "good doctor" characteristics included: excellence in communication and leadership, empathy, altruism, and clinical competence. Motivating factors for the "good doctor" in the ICU included high acuity with high degree of satisfaction with positive patient outcomes, as well as the opportunity to build relationships with families during difficult times. Barriers included system limitations (e.g. resources, documentation, administrative tasks) as well as time-constraints. Clinicians highlighted the importance of clear and honest communication in an ideal clinician-family relationship.Obstacles to that relationship included time limitations which can prevent understanding families’ values as well as competing interests between patient safety relative to parental perceptions of comfort.
Conclusion(s): Both clinicians and families are aligned in ideals that promote children’s health and prevent suffering through open and honest communication. Time constraints and misunderstanding of caregiver priorities is a barrier to successful alignment. Clinician training to improve empathetic communication is essential to providing quality patient care that supports families aims of good parents. It is important to next examine the parental perspective of the "good doctor" to further align perspectives of clinicians and families.
The "Good Doctor"
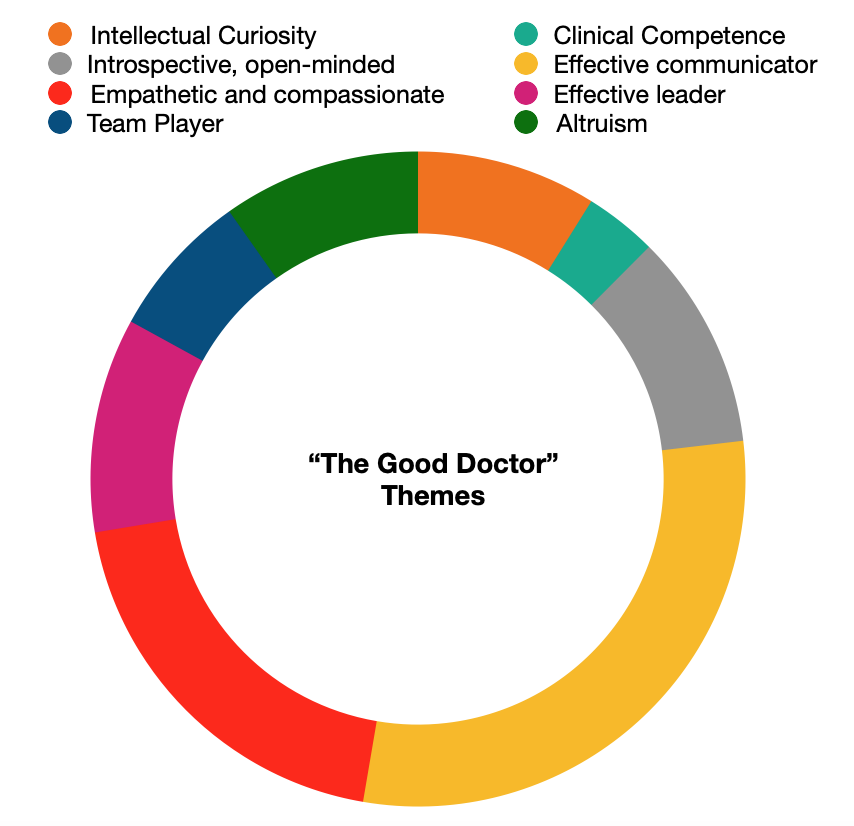 Clinician themes of "good doctor" characteristics qualitatively defined by ICU providers.
Clinician themes of "good doctor" characteristics qualitatively defined by ICU providers. 
