Critical Care 2
Session: Critical Care 2
123 - COVID19 and Enrollment of Critically Ill Children in a Clinical Trial
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 123.4236
Sarah B.. Kandil, Yale School of Medicine, New Haven, CT, United States; David J. Panisello-Manterola, Yale-New Haven Children's Hospital, Elmira, NY, United States; Madhuradhar Chegondi, University of Illinois College of Medicine, Peoria, IL, United States; Christine Allen, Oklahoma Childrens Hospital at OU Health, Oklahoma City, OK, United States; Jill M. Cholette, Golisano Children's Hospital at The University of Rochester Medical Center, Rochester, NY, United States; Michele Kong, University of Alabama School of Medicine, Birmingham, AL, United States; Matthew Pinto, Maria Fareri Children's Hospital at Westchester Medical Center, Valhalla, NY, United States; E Vincent Faustino, Yale School of Medicine, New Haven, CT, United States; Christie L. Glau, Perelman School of Medicine at the University of Pennsylvania, Newtown Square, PA, United States; Hilary Schreiber, Children's Hospital of Wisconsin, Milwaukee, WI, United States
- SK
Sarah B. Kandil, MD (she/her/hers)
Associate Professor of Pediatrics, Critical Care Medicine
Yale School of Medicine
New Haven, Connecticut, United States
Presenting Author(s)
Background: Enrollment of critically ill children in randomized clinical trials (RCT) is challenging. Rising in prevalence during the coronavirus-19 (COVID19) pandemic, science denialism has further complicated enrollment.
Objective: We hypothesized that the COVID19 pandemic is associated with lower enrollment rates of critically ill children in RCTs due to increased parental refusal.
Design/Methods: We enrolled in 5 centers a phase 2b RCT of early prophylaxis against catheter-associated thrombosis in critically ill children from November 2017 to August 2019 (pre-COVID19). We randomized critically ill children < 18 years old with a newly inserted central venous catheter to enoxaparin prophylaxis or usual care. Based on findings from this RCT, enrollment for a multicenter (15 centers) phase 2/3 RCT with comparable eligibility criteria and study design began in May 2022 (post-COVID19). In this study, we analyzed eligible children from the pre-COVID19 RCT and up to August 2024 from the post-COVID19 RCT. Enrollment rates and reasons for failure to enroll were analyzed with descriptive statistics and Chi-Squared analysis.
Results: We analyzed 622 eligible children, of whom 165 (26.5%) were pre-COVID19 and 457 (73.5%) were post-COVID19. Enrollment rates were 30.9% pre-COVID19 and 18.2% post-COVID19 (P=0.001). Distribution of reasons for not enrolling eligible children were different pre- and post-COVID19 (P=0.001) (Figure 1). Parents not available was proportionally lower post-COVID19 (17.7% vs 34.2% pre-COVID19, P< 0.001), while research staff not available was higher post-COVID19 (28.6% vs 15.8% pre-COVID19, P=0.006). Parental refusal was comparable (38.6% pre-COVID19 vs 39.6% post-COVID19, P=0.85). However, the percentage of parental refusal per hospital was inversely correlated with the percentage of research staff not available (correlation coefficient: –0.71, P=0.003) (Figure 2). Among all eligible patients, enrollment failure due to the percentage of parental refusal was higher post-COVID19 at 64.1% of 231 children versus 46.3% of 95 children pre-COVID19 (P=0.003) (Figure 3).
Conclusion(s): The COVID19 pandemic is associated with lower enrollment rates of critically ill children in RCTs. In children approached for RCT enrollment, the percentage of parental refusal was more frequent post-COVID19. This is confounded by higher rates of research staff not available post-COVID19. Further studies should explore the impact of science denialism in parental refusal to identify interventions and increase enrollment of critically ill children in RCTs.
Figure 1
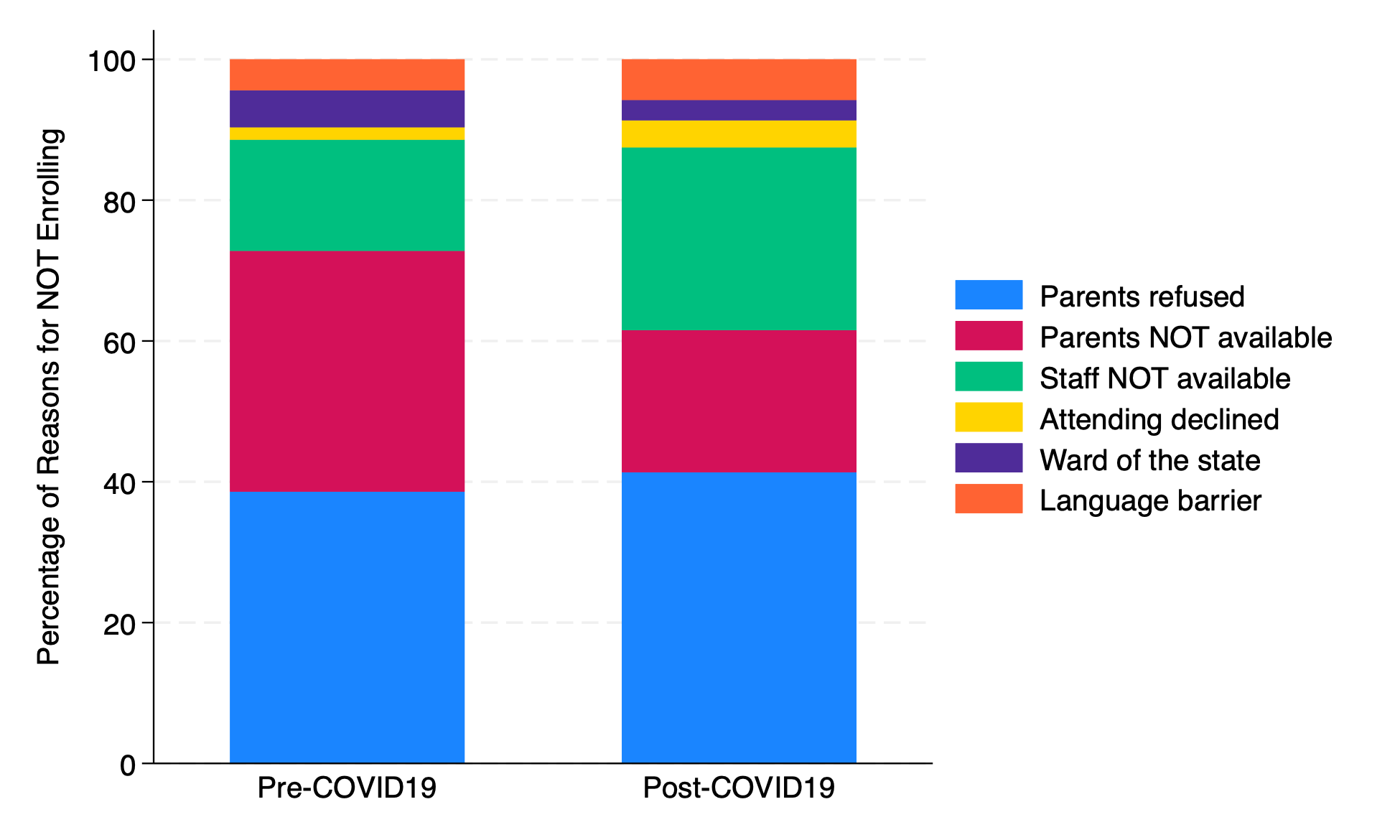 Stacked bar chart of reasons for not enrolling eligible children by enrollment period. The distribution of reasons for not enrolling these children was different pre- and post-COVID19.
Stacked bar chart of reasons for not enrolling eligible children by enrollment period. The distribution of reasons for not enrolling these children was different pre- and post-COVID19. Figure 2
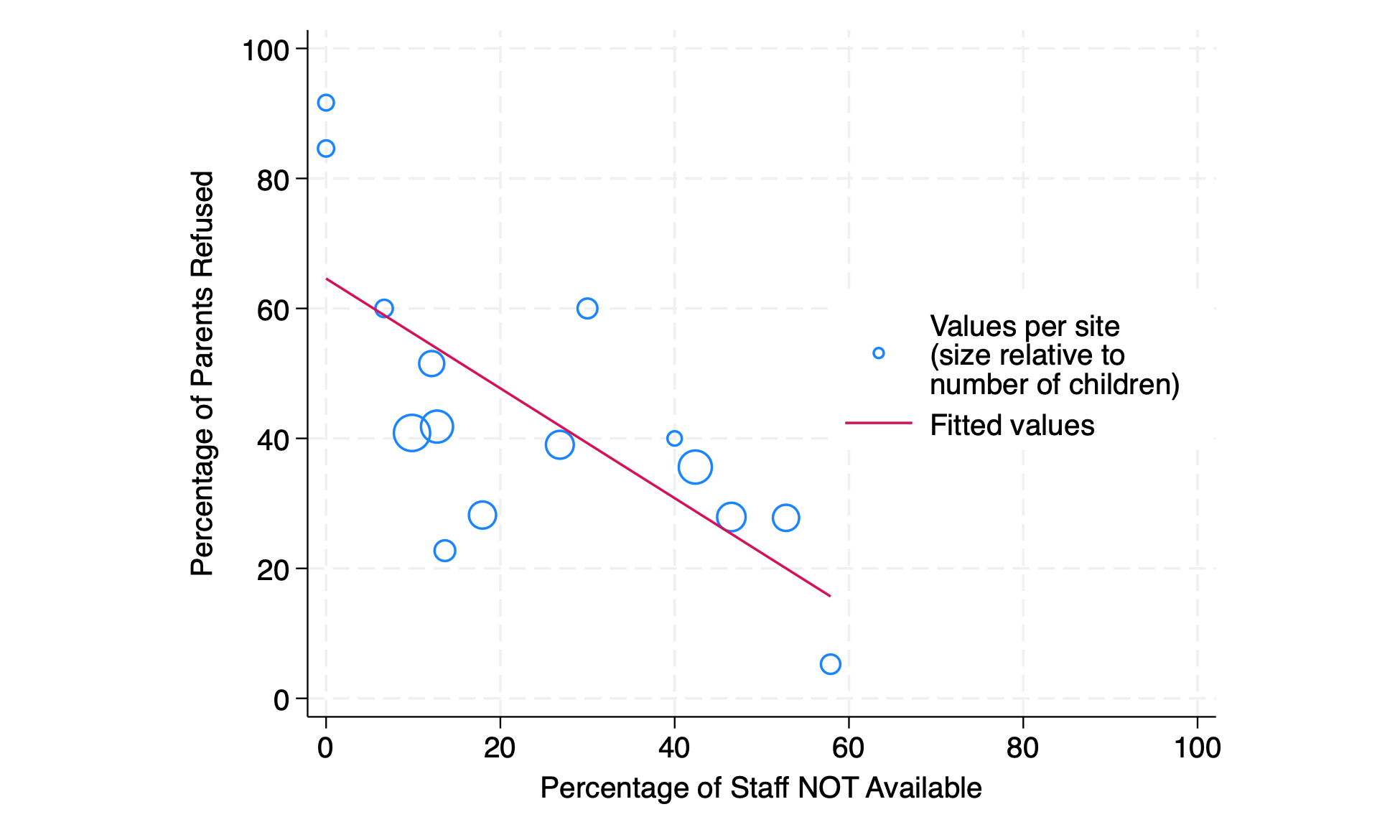 Scatterplot of parental refusal and research staff not available. The percentage of parental refusal per hospital was inversely correlated with the percentage of unavailability of research staff.
Scatterplot of parental refusal and research staff not available. The percentage of parental refusal per hospital was inversely correlated with the percentage of unavailability of research staff.Figure 3
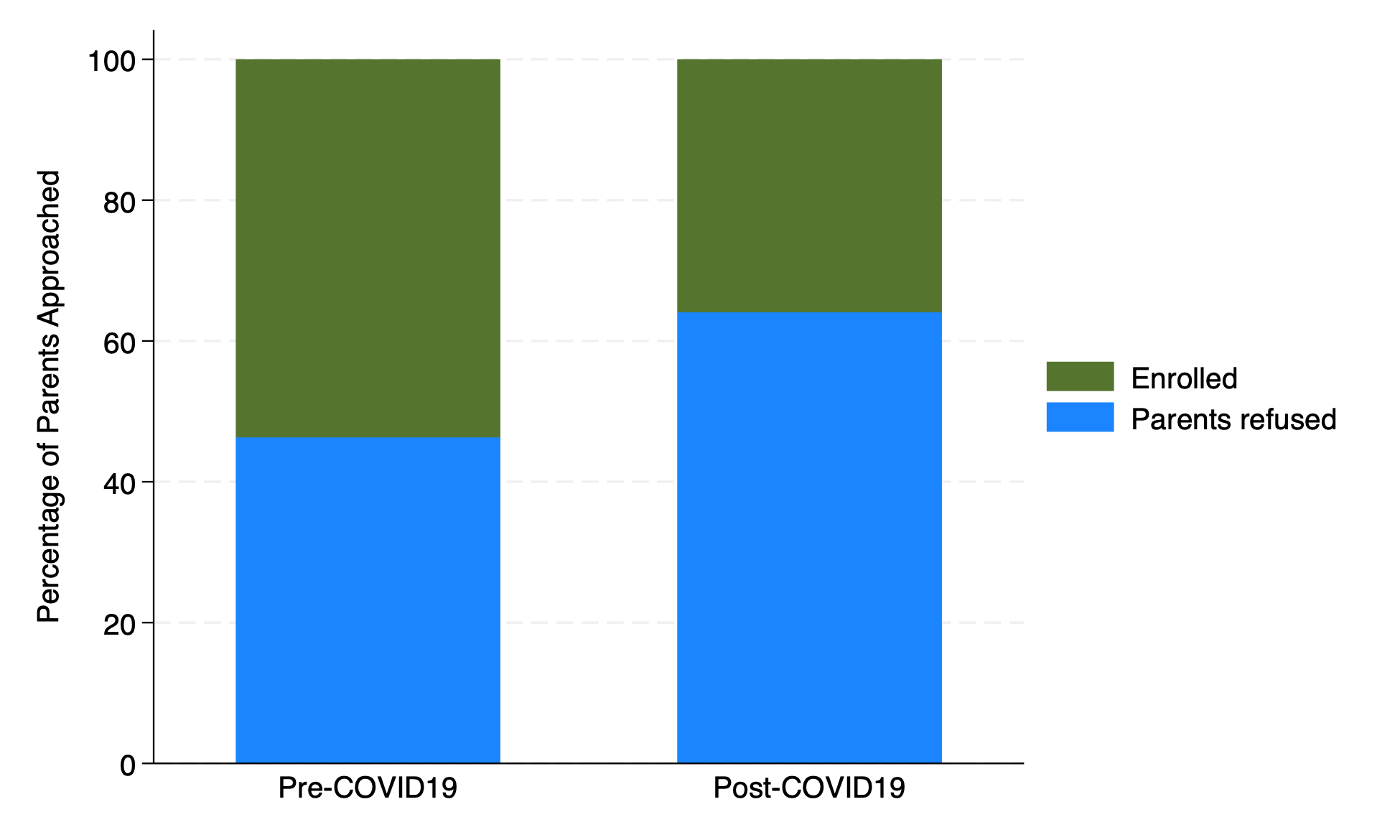 Stacked bar chart of outcomes of parents approached for enrollment. Among these children, the percentage of parental refusal was higher post-COVID19 than pre-COVID19.
Stacked bar chart of outcomes of parents approached for enrollment. Among these children, the percentage of parental refusal was higher post-COVID19 than pre-COVID19.
