Neonatal Quality Improvement 1
Session: Neonatal Quality Improvement 1
061 - Initiating Infant Driven Feeding In A Level 3 Community NICU, A Quality Improvement Project
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 61.5437
Tatyana Kopp, New York Presbyterian-Queens, Woodmere, NY, United States; Angela Melkonian, New York Presbyterian- Queens, Flushing, NY, United States; Kalliope Tsirilakis, Weill Cornell Medicine, Fresh Meadows, NY, United States; Natasha Cruz-Vicente, New York Presbyterian Queens, Jamaica, NY, United States; Chyong-Yunn Chang, New york presbyterian, Flushing, NY, United States; Thaydene Samuels, New York Presbyterian, Deer Park, NY, United States
- TK
Tatyana Kopp, DO (she/her/hers)
Director of Quality and Patient Safety, Inpatient Pediatrics
New York Presbyterian-Queens
Woodmere, New York, United States
Presenting Author(s)
Background: Difficulty transitioning to oral feeding is common in premature infants and can prolong NICU length of stay (LOS) (1). The Infant Driven FeedingTM (IDF™) program provides a standardized, developmentally supportive pathway for initiation and advancement of oral feeds in the NICU. Standardized cue-based feeding protocols have been associated with shortened transition time to full oral feeding (2,3).
Objective: To successfully implement IDF™ in the NICU by achieving >90% Readiness Score documentation, Quality Score documentation, and accurate Quality Scoring by February 2025.
Design/Methods: This is an observational time series study using the model for improvement and planned experimentation to test interventions designed to improve oral feeding methods in the NICU. Nursing education was completed as provided by Dr. Brown’s™ with pre and post-test data collected. IDF™ was initiated in February 2023. Unit support was provided by SLP, nursing, and physician project champions. EMR smart phrases were created for documentation of IDF™ and a mnemonic to help the clinical and nursing team remember which infants qualified for IDF™ scoring. Chart reviews were performed to collect implementation data and 4 PDSA cycles have since been completed including educational huddles, reference cards, and re-education via the IDF™ learning platform.
Results: Nursing pre and post-test knowledge scores showed improvement, average scores of 56% to 87% respectively. Our chart review looked at three main components of IDF™ implementation; Readiness Score documentation, Quality Score documentation, and the accuracy of the Quality Scores being documented. An improvement was seen in all three categories with consecutive PDSA cycles (Fig. 1, 2 ,3).
Conclusion(s): The first two PDSA cycles demonstrated stability in two key components of program implementation while highlighting accuracy of Quality Scores documented as an initial area of opportunity. With continued efforts there has been improvement in all three process measures. Consistent with the literature (3), successful implementation requires time, ongoing interdisciplinary support, and re-education to supplement initial staff-wide training. A recently awarded grant will fund further staff education which is anticipated to help improve compliance and accuracy of implementation. A future goal will be to show improved LOS in the NICU through IDF™ implementation.
Fig. 1 IDF Readiness Score Documentation
.jpg) Percentage of feeding intervals with documented IDF Readiness Scores.
Percentage of feeding intervals with documented IDF Readiness Scores. Fig. 2 IDF Quality Score Documentation
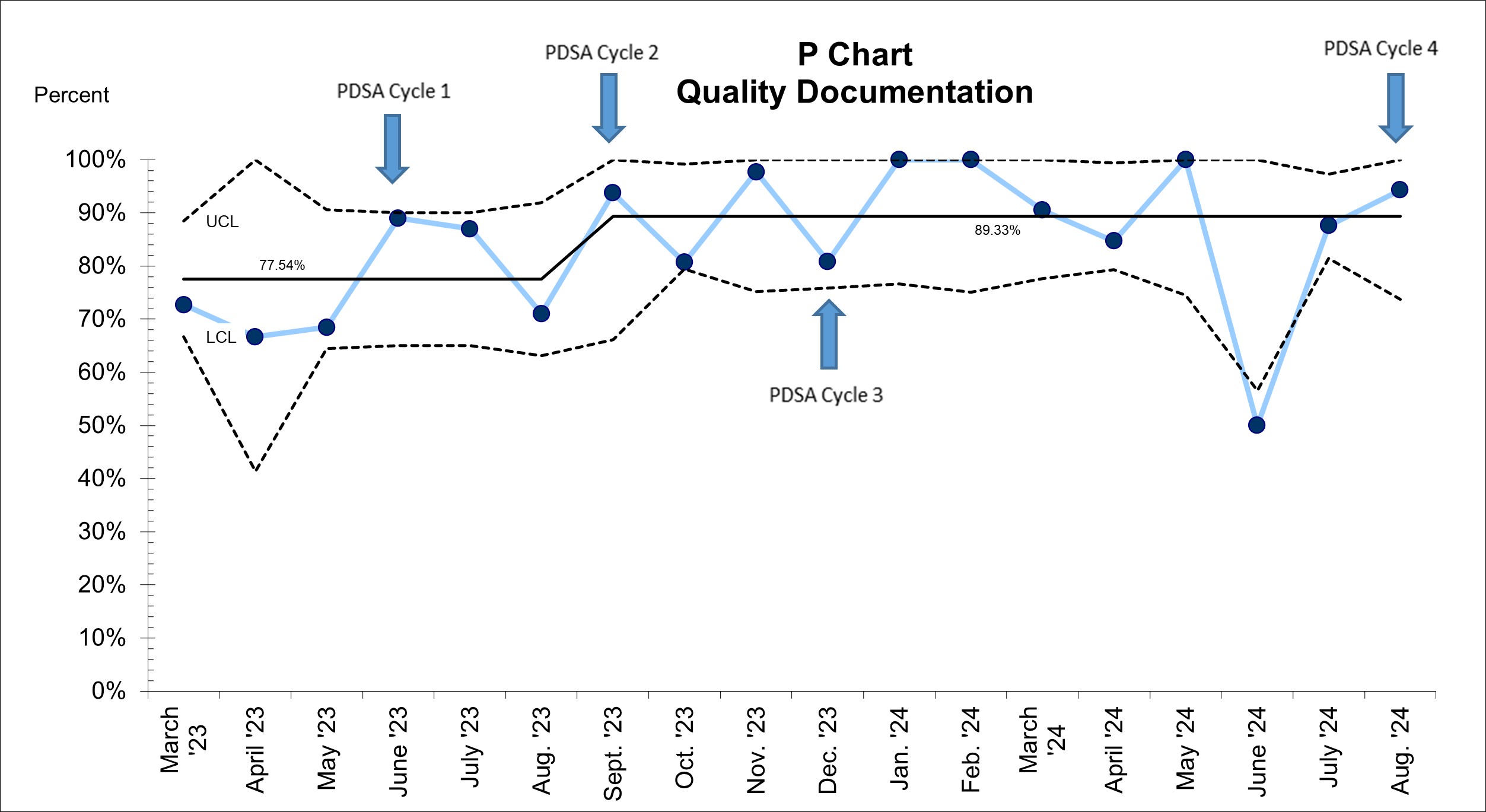 Percentage of oral feeds with documented IDF Quality scores.
Percentage of oral feeds with documented IDF Quality scores. Fig. 3 IDF Quality Score Accuracy
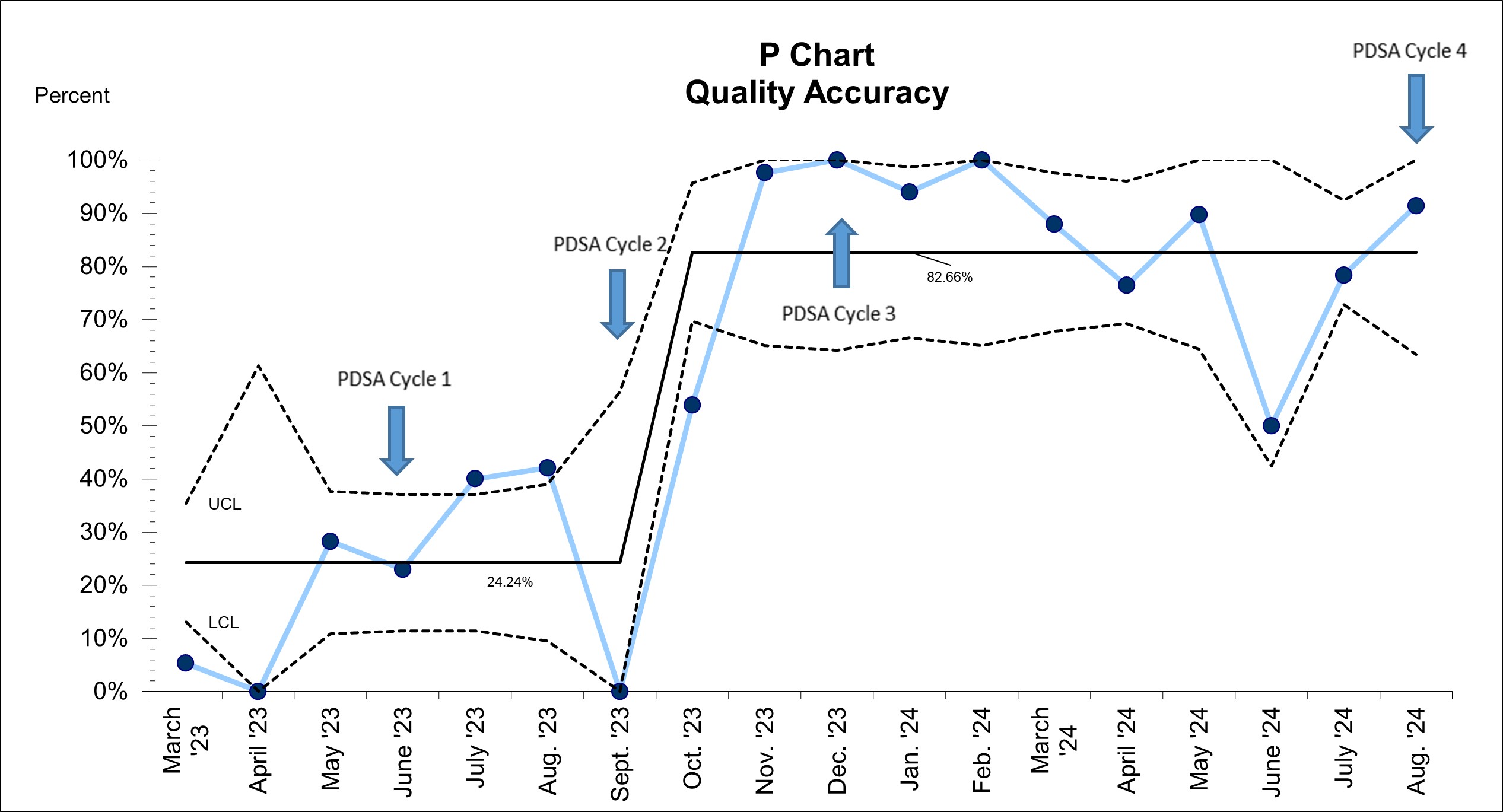 Percentage of documented IDF Quality Scores that were determined and documented accurately.
Percentage of documented IDF Quality Scores that were determined and documented accurately. 

