Neonatal Quality Improvement 1
Session: Neonatal Quality Improvement 1
056 - Implementation of a structured "Keep the PEEP" Bundle to Reduce Extubation Failure in Preterm Infants
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 56.5414
Sandra L. Leibel, University of California, San Diego School of Medicine, San Marcos, CA, United States; Lauren A. Suh, University of California, San Diego School of Medicine, San Diego, CA, United States; Audra Wise, Pediatrix, Las Vegas, NV, United States; Katherine Weiss, Rady Children's Hospital San Diego, OCEANSIDE, CA, United States
Sandra L. Leibel, MD MS (she/her/hers)
Associate Professor
University of California, San Diego School of Medicine
San Marcos, California, United States
Presenting Author(s)
Background: Preterm infants often require invasive positive pressure ventilation (PPV). Failure to maintain these infants on non-invasive support (NIS) after extubation contributes to an increased risk of developing bronchopulmonary dysplasia (BPD).
Objective: Our SMART aim was to reduce the rate of re-intubation within 72 hours of extubation by 30% and decrease the mean number of ventilator days by 20% for infants born at < 30 weeks GA or weighing < 1500 grams in the NICU over a year and a half. Our Global aim was to decrease the incidence of BPD in preterm infants by improving post-extubation respiratory support practices.
Design/Methods: This 1.5 year quality improvement (QI) initiative involved a multidisciplinary team using a Key Driver Diagram and Fishbone Analysis, leading to the development of a structured “Keep the PEEP” (KTP) bundle, implemented through Plan-Do-Study-Action (PDSA) cycles. The first cycle focused on creating algorithms and summary cards for respiratory therapists and nurses to troubleshoot infants on CPAP independently, establishing checklists to monitor clinical stability on CPAP, and standardizing nasal barriers for babies on F&P CPAP. The second cycle implemented intubation/extubation guidelines and order sets for physicians and nurse practitioners to standardize decisions on invasive ventilation. The third aim was to implement the bundle in community delivery hospitals that admit and care for preterm infants. The checklists were collected weekly to confirm adherence, while order sets and patient outcomes after extubation were monitored monthly through the EMR. The Outcome Measure was the rate of extubation failure, defined as re-intubation within 72 hours of extubation. The Process Measure was compliance with the KTP bundle components. The Balancing Measure was the incidence of nasal trauma or skin breakdown related to CPAP.
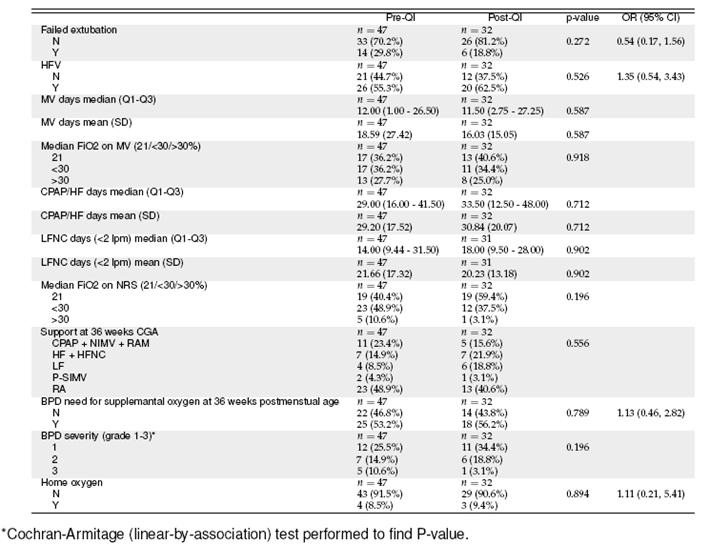
Results: The initiative achieved its SMART aims, reducing extubation failure by 47% and reducing the mean number of days on mechanical ventilation by 33%. Although there was no reduction in overall BPD, a 79% reduction in severe BPD was achieved.
Conclusion(s): This QI initiative effectively reduced extubation failure rates and ventilator days in preterm infants. Further trials, including a standardized CPAP weaning algorithm, are planned to reduce variability in NIS use and optimize lung-protective strategies post-extubation.
NICU Respiratory Interventions and Outcomes
Extubation Failure Rates - Run Chart
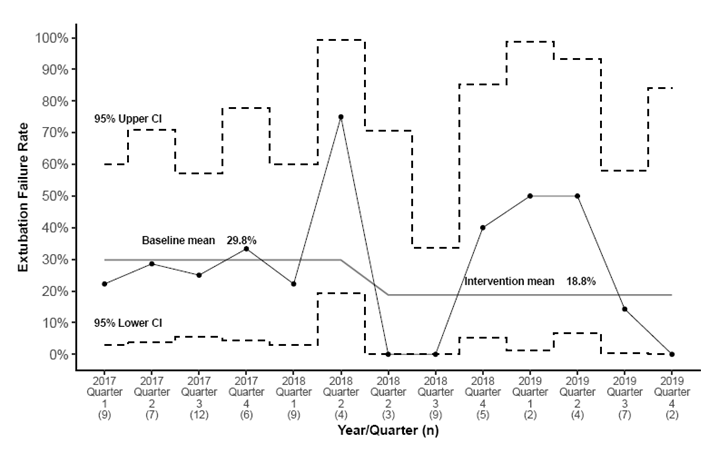 QI intervention begins in 2018 Quarter 2 (second one).
QI intervention begins in 2018 Quarter 2 (second one).Mean Number of Ventilator Days - Run Chart
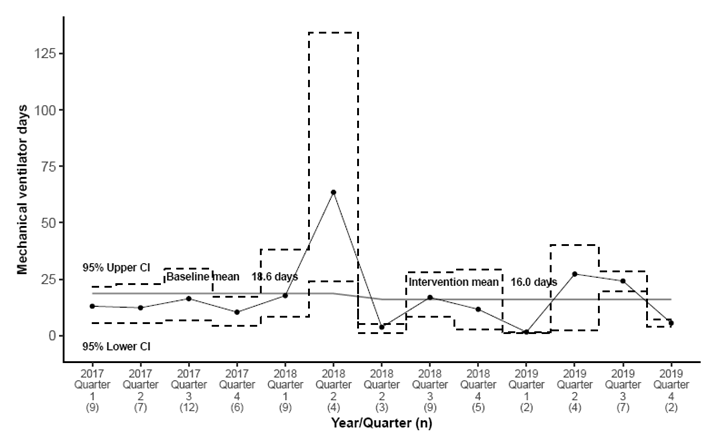 QI intervention begins in 2018 Quarter 2 (second one).
QI intervention begins in 2018 Quarter 2 (second one).

