Emergency Medicine 2
Session: Emergency Medicine 2
429 - Paediatric trauma inter-hospital retrieval: A 10-year review of patient outcomes in New South Wales, Australia
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 429.5937
Michael McCarron, Newborn and Paediatric Emergency Transport Service, NSW, Surry Hills, New South Wales, Australia; Kathryn A. Carmo, Sydney Children's Hospitals Network, BANKSTOWN AERODROME, New South Wales, Australia; Soundappan S V Soundappan, Children's Hospital at Westmead, Sydney, New South Wales, Australia

Michael McCarron, MBChB MRCPCH FRACP (he/him/his)
Paediatric Retrieval Consultant
Newborn and Paediatric Emergency Transport Service, NSW
Surry Hills, New South Wales, Australia
Presenting Author(s)
Background: Six percent of the 4000 admitted major trauma cases in New South Wales (NSW) hospitals were children in 2019-2020. With only 3 Paediatric Trauma Centres (PTC), nearly half of Paediatric major trauma cases require inter-hospital retrieval. The Newborn and Paediatric Emergency Transport Service (NETS) is a specialist service providing clinical advice and critical care retrieval across the state. There have been no large studies comparing the time taken by paediatric retrieval teams and adult medical retrieval services (AMRS) to stabilise patients and overall transport time to a PTC in Australia.
Objective: To compare time taken to retrieve patients to a PTC; in-hospital morbidity; and mortality between NETS and AMRS teams.
Design/Methods: This is a retrospective observational study of trauma patients aged 0-15 years referred to the NETS clinical co-ordination centre who were retrieved or transported to a PTC between 1 January 2009 and 31 December 2019. Demographic and referral data were obtained from the prospectively completed NETS database. Data was linked with patient electronic medical records at each of the 3 PTCs for follow up data on injury severity score (ISS), intensive care unit (ICU) and total hospital length of stay (LOS), and mortality outcomes. Exclusions from this study are detailed in figure 1.
Results: Two-thousand eight-hundred and twenty-four cases were identified (figure 1) with 1702 cases included for PTC follow up data collection. Seven-hundred and seventy-two cases were excluded. Of the 932 retrievals included, NETS retrieved 427, AMRS teams 109, paramedics or flight nurses 356 and a regional paediatric team retrieved 40. The mean ISS was 14 for medical retrievals, and 9 for paramedic/flight nurses. The median time from tasking to completion of retrieval by NETS was 233 minutes, IQR 163-371 minutes; and by AMRS 262 minutes, IQR 210-361 minutes (p=0.09). Forty-one percent of patients were admitted to ICU. The odds of ICU showed no difference between AMRS and NETS (OR 1.003, 95%CI 0.63-1.59, p=0.99) (Table 1). There was no difference in median length of hospital LOS between NETS (5 days, IQR 2-10); and AMRS (5 days, IQR 3-13), p=0.34 (Table 2). Twenty-two patients in the study died. There was no significant difference between NETS and AMRS.
Conclusion(s): Paediatric retrieval teams complete most inter-hospital retrievals to a PTC. This large study shows that there is no significant difference between NETS and AMRS for retrieval times, major morbidity and mortality outcomes for paediatric trauma retrievals. Further studies should explore differences in care provided by transport providers.
Figure 1: Study participant flow diagram
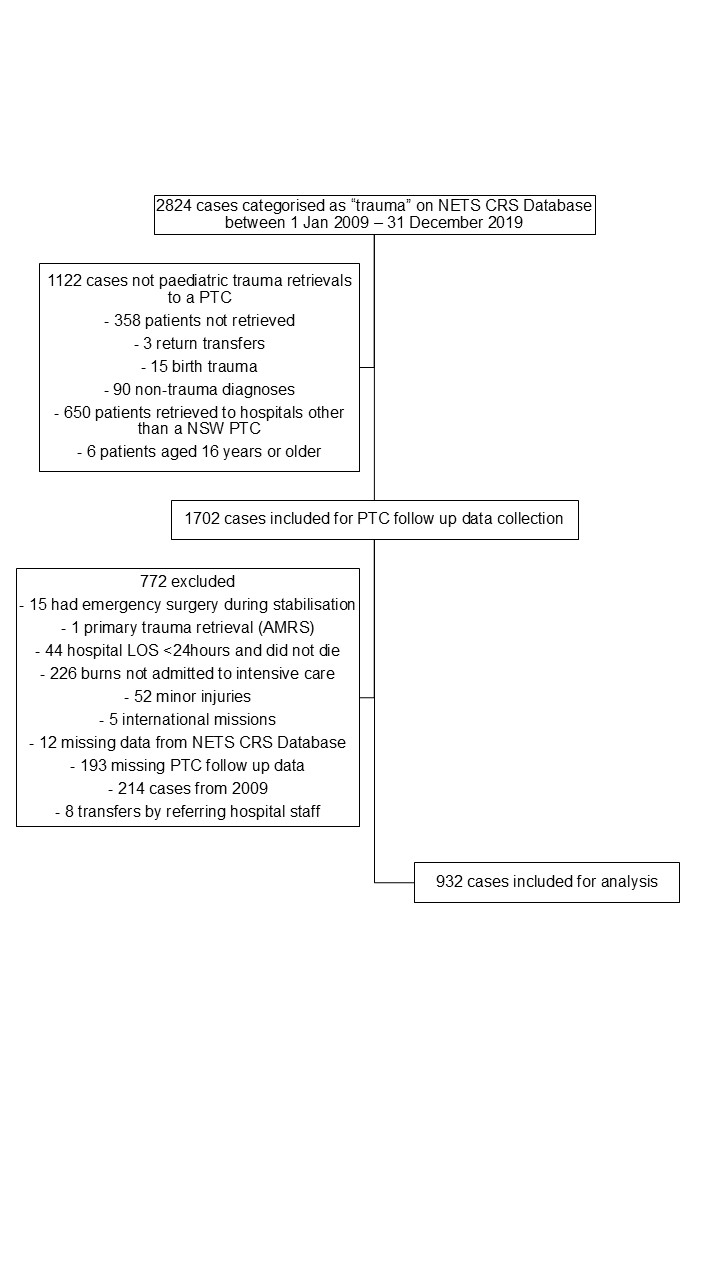
Table 1: Intensive Care Unit (ICU) admission frequency and Length of Stay (LOS) by retrieval team
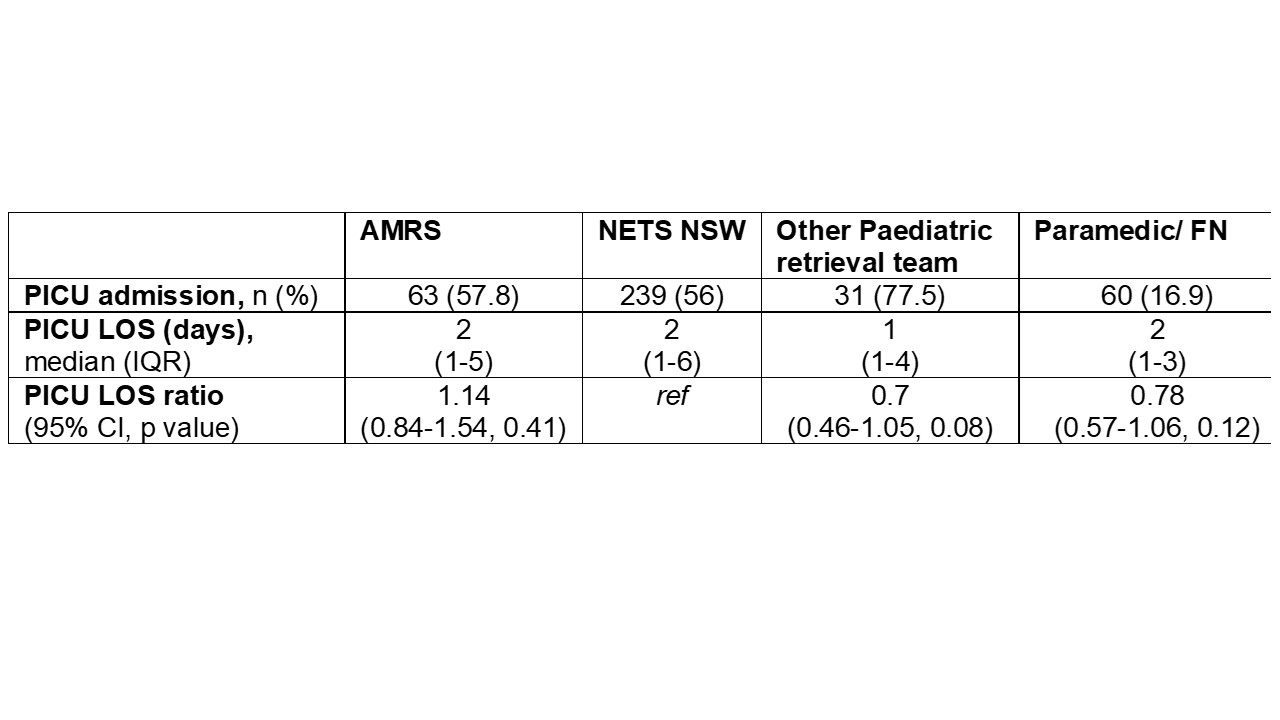
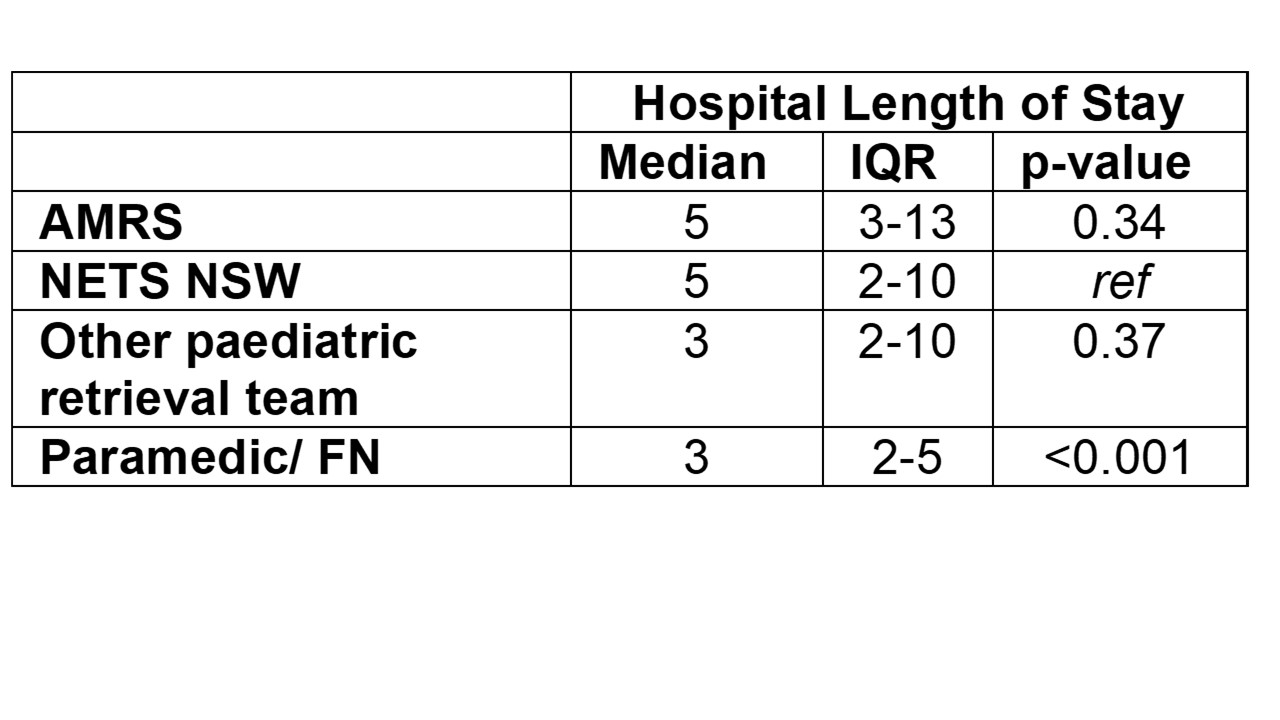
Table 2: Hospital length of stay (LOS) by retrieval team