Neonatal/Infant Resuscitation 2
Session: Neonatal/Infant Resuscitation 2
295 - Knowledge, attitude, and practices (KAP) regarding use of supraglottic airways during neonatal resuscitation: survey among nurses in community and university hospitals
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 295.5646
Jessa Rose A. Li, University of California Davis Children's Hospital, Sacramento, CA, United States; Janelle Beall, University of California Davis Children's Hospital, Sacramento, CA, United States; Evan M. Giusto, UC Davis Health, Sacramento, CA, United States; Satyan Lakshminrusimha, UC Davis, Sacramento, CA, United States; Deepika Sankaran, University of California Davis Children's Hospital, Sacramento, CA, United States

Jessa Rose A. Li, BS, MD (she/her/hers)
Pediatric Resident
University of California Davis Children's Hospital
Sacramento, California, United States
Presenting Author(s)
Background: Positive pressure ventilation (PPV) is the most important component of neonatal resuscitation. Current NRP guidelines recommend initiating PPV using a neonatal facemask and if the baby cannot be successfully ventilated with a face mask and intubation is not feasible or unsuccessful, a laryngeal mask airway (LMA) may provide a successful rescue airway. However, the use of an LMA remains infrequent among neonatal providers. A recent article by Zaichkin et al advocates for “empowering nurses in the use of LMA during neonatal resuscitation”. Unfortunately, there is a lack of data on the use of LMA by neonatal registered nurses (RNs). Increasing the use of LMA by NICU RNs may improve resuscitation outcomes in communities without ready access to neonatal physicians.
Objective: To evaluate the KAP on and barriers to LMA use during neonatal resuscitation among neonatal RNs in university and community hospitals.
Design/Methods: A questionnaire that was developed based on input from neonatal clinicians and RNs which included questions on demographics, experience and confidence in the use of LMA, and perceived barriers in LMA use during neonatal resuscitation. The anonymous questionnaire was disseminated to neonatal RNs in four community hospitals and one university hospital in the Greater Sacramento area.
Results: Responses from 38 RNs from the university hospital and 94 RNs from the community hospital neonatal intensive care units (NICU) were collected and analyzed. Fewer RNs from university hospitals (68%) have had training in LMA placement compared to those from community hospitals (82%). RNs from the university center (24%) placed more LMAs in live newborns compared to community centers (17%); however, this was not statistically significant (p-value=0.11) (Table 1). The most common barrier for LMA use was preference for ETT placement (63%) and lack of experience (55%) for university and community hospital RNs, respectively (Image 1).
Conclusion(s): The highest perceived barrier for LMA placement differed between NICU RNs from university and community hospitals. To further understand the factors contributing to the current practice, we will conduct small focus group interviews to help facilitate understanding of supraglottic airway use among RNs in university and community NICUs.
Table 1
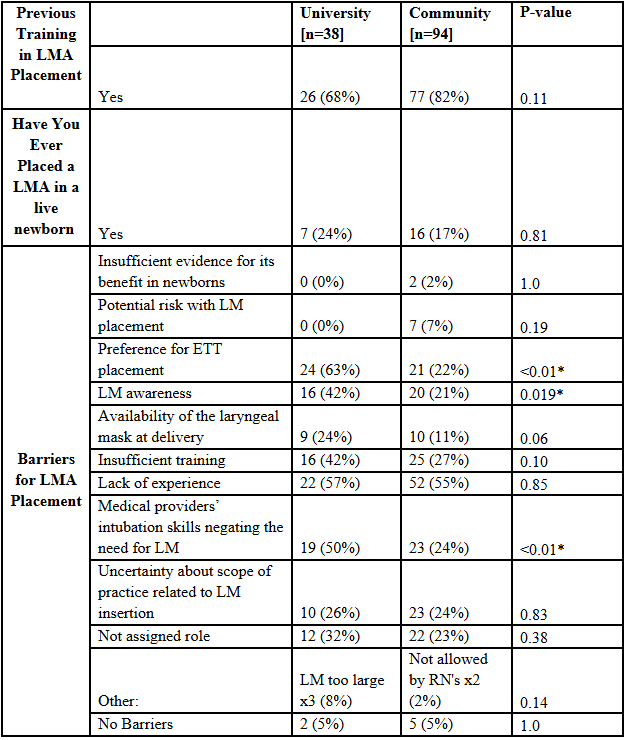 Questionnaire data depicting NICU RNs university versus community hospital responses. P-value < 0.05 is considered significant, which is indicated with an *.
Questionnaire data depicting NICU RNs university versus community hospital responses. P-value < 0.05 is considered significant, which is indicated with an *.Image 1
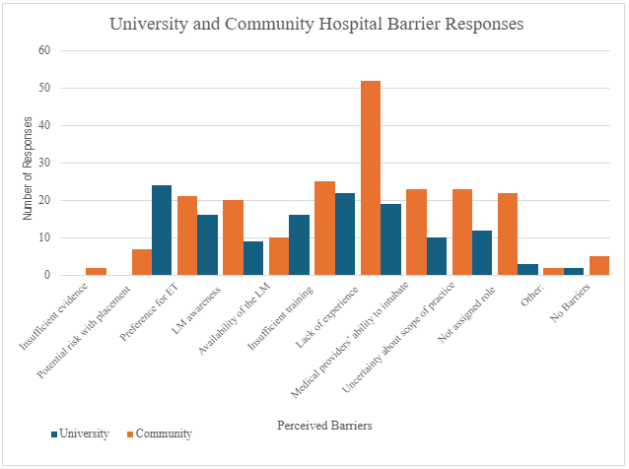 University verses community hospital responses to perceived barriers in LMA use during neonatal resuscitation.
University verses community hospital responses to perceived barriers in LMA use during neonatal resuscitation.Table 1
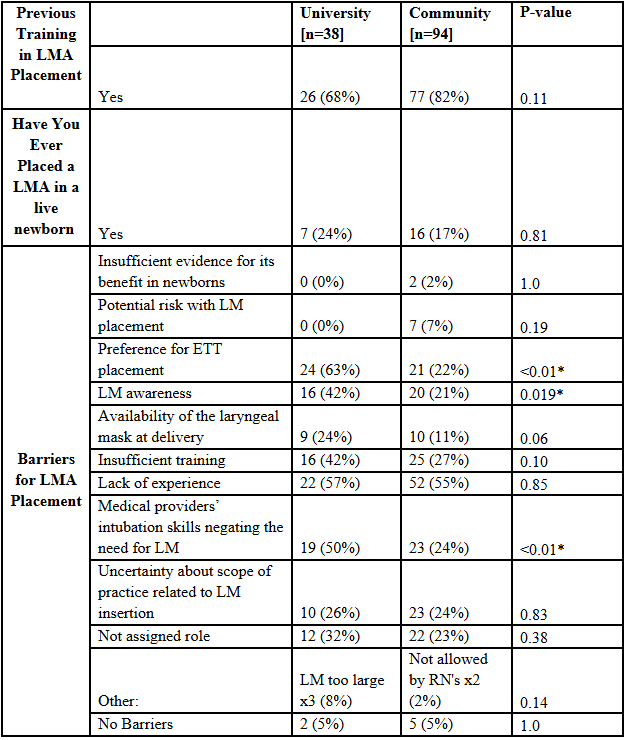 Questionnaire data depicting NICU RNs university versus community hospital responses. P-value < 0.05 is considered significant, which is indicated with an *.
Questionnaire data depicting NICU RNs university versus community hospital responses. P-value < 0.05 is considered significant, which is indicated with an *.Image 1
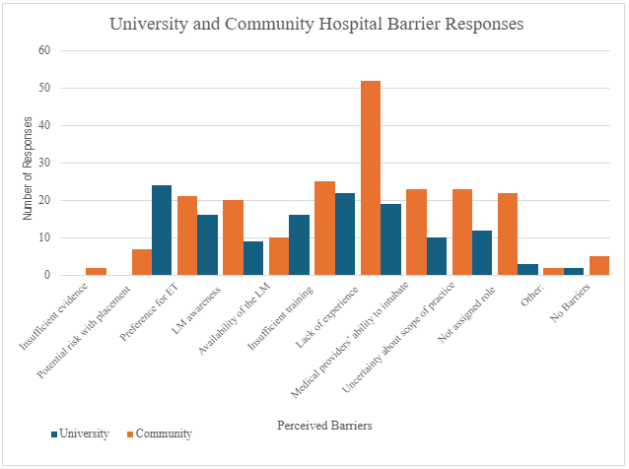 University verses community hospital responses to perceived barriers in LMA use during neonatal resuscitation.
University verses community hospital responses to perceived barriers in LMA use during neonatal resuscitation.
