Neonatal Neurology 3
Session: Neonatal Neurology 3
373 - Neonatal Sequential Organ Failure Assessment Scores to Predict Neurological Outcomes of Infants Diagnosed with Hypoxic-Ischemic Encephalopathy
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 373.5760
Kaitlyn S. Lagnese, University of Florida College of Medicine, Gainesville, FL, United States; dhanashree Rajderkar, University of Florida, Gainesville, FL, United States; Juan C.. Roig, University of Florida, Gainesville, Gainesville, FL, United States; James L. Wynn, University of Florida College of Medicine, Gainesville, FL, United States; Michael D. Weiss, University of Florida College of Medicine, Gainesville, FL, United States

Kaitlyn S. Lagnese, DO (she/her/hers)
Fellow of Neonatal-Perinatal Medicine
University of Florida College of Medicine
Gainesville, Florida, United States
Presenting Author(s)
Background: Identification of neurodevelopmental impairment (NDI) risk early after birth among neonates with hypoxic-ischemic encephalopathy (HI) that receive therapeutic hypothermia (TH) is a critical antecedent to improvement of care and precision medicine.
Objective: Determine the relationship between early critical organ dysfunction and NDI among neonates diagnosed with HI that receive TH.
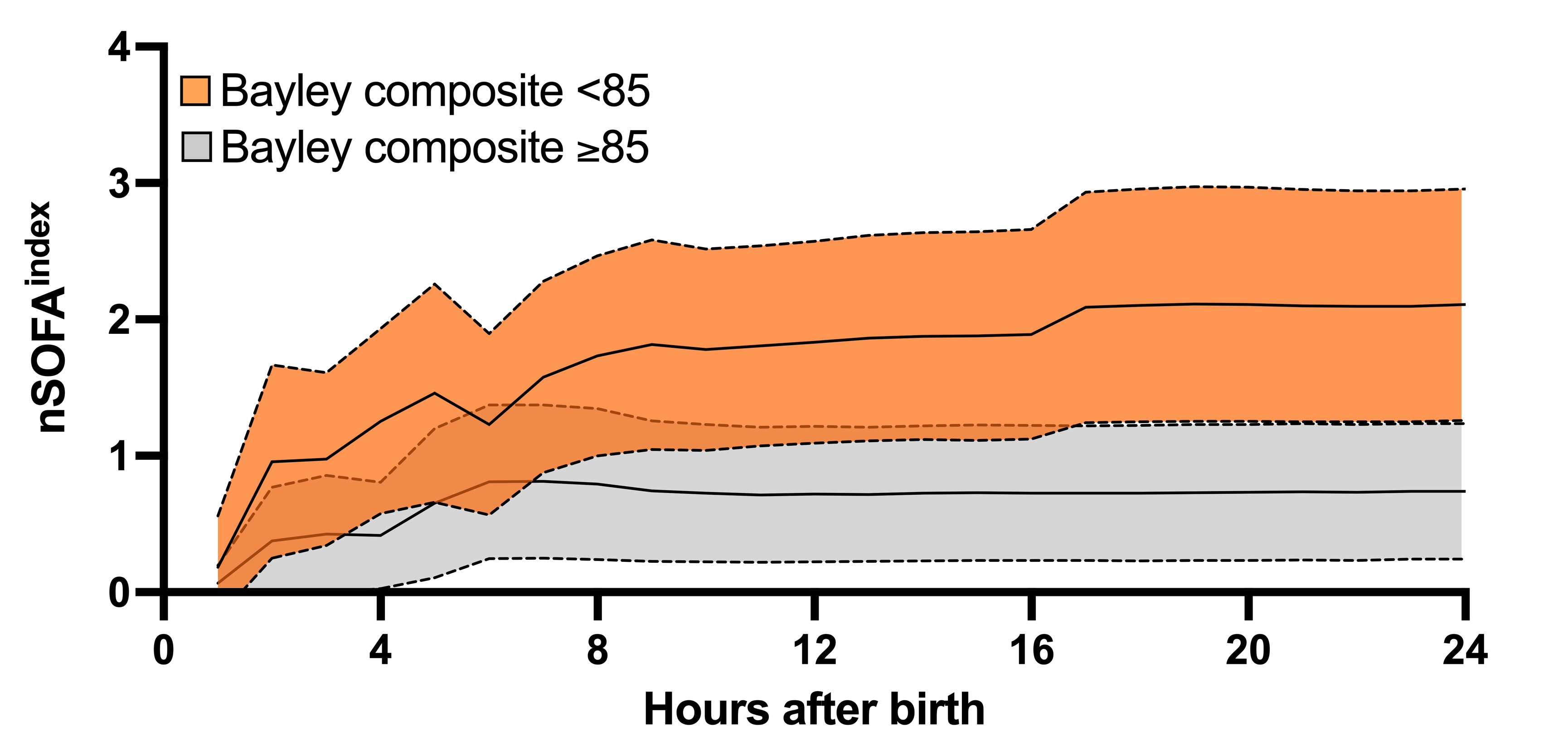
Design/Methods: After IRB approval, we performed a single-center, retrospective cohort study of neonates admitted to UF Health NICU from 1/2012 to 4/2023 who received TH and had a Bayley Scales of Infant and Toddler Development assessment between 15 and 24 months of age. An integrated data repository (IDR) containing all electronic health record data was created and utilized for this work. Hourly neonatal sequential organ failure assessment (nSOFA) scores were calculated for all patients from admission to discharge using the IDR. The average nSOFA score by hour after birth (nSOFA index) at selected timepoints were compared between those with Bayley composite score < 85 (NDI) and those ≥85 (no NDI). All routine clinical laboratory test values were also analyzed. Statistical testing was done based on data type and distribution with significance set at p< 0.05. Area under the receiver operating characteristic (AUROC) curve and a multivariable linear regression (MVLR) model were applied.
Results: 89 infants met study criteria. NDI occurred in 45/89 (51%). Differences between groups (no NDI and NDI) were present in median 5-minute Apgar (5 (4, 7) vs 4 (2, 6), p =0.007), outborn status (35% vs 65%, p=0.03), and median length of stay (days) (12 (8, 16) vs 21 (IQR 9, 36), p=0.006). The mean minimum platelet count showed the greatest difference among lab results between groups within 12 hours of birth (210x10^3 (SD 52x10^3) vs 175x10^3 (72x10^3), p=0.009) and remained significant 12-24 hours after birth (195x10^3 (61x10^3) vs 165x10^3 (57x10^3), p=0.02). Comparisons of hourly nSOFA index values within 24 hours after birth were significantly and continuously different (p < 0.05) between no NDI and NDI groups from 7 to 24 HOL (Figure 1). A MVLR model (5-minute Apgar score, outborn, maximum nSOFA index within 24 hours of birth, and the minimum platelet count within 12 hours of birth yielded an AUROC of 0.74 for NDI (95%CI 0.63, 0.84, p< 0.0002); NPV 66.0%, PPV 69.1%.
Conclusion(s): Using routinely collected data including the nSOFA, we found good discrimination ability for NDI at 15-24 months among HI patients that received TH. These results may improve precision strategies and modify enrollment in clinical trials.
Average nSOFA (nSOFA index) by hour after birth among neonates with hypoxic-ischemic encephalopathy that received therapeutic hypothermia