Quality Improvement/Patient Safety 5
Session: Quality Improvement/Patient Safety 5
476 - Improving Normothermia Post-Operatively at the Level IV NICU
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 476.5413
Tetyana H. Nesterenko, University of Texas Southwestern Medical School, Dallas, TX, United States; Rebecca Palmer, Children's Health, Dallas, TX, United States; Sushmita Yallapragada, University of Texas Southwestern Medical School, Dallas, TX, United States; Alissa Doll, University of Texas Southwestern Medical Center, Dallas, TX, United States; Brenna Kelly Brenna Kelly, child, Dallas, TX, United States; Kymeyone Lanehart, Kym Lanehart - Children's Health Dallas, Forney, TX, United States; Katie A. Liu, University of Texas Southwestern Medical School, Dallas, TX, United States; Jami E. Miller, Children's Health - - Dallas, TX, Dallas, TX, United States; Charmaine Shaw, Children’s Dallas, Forney, TX, United States; Jerithea Tidwell, Children's Health Dallas, Dallas, TX, United States

Tetyana H. Nesterenko, MD, MSHS (she/her/hers)
Medical Director, Quality and Safety
University of Texas Southwestern Medical School
Dallas, Texas, United States
Presenting Author(s)
Background: Neonates in the NICU are highly susceptible to perioperative hypothermia, a condition linked to increased morbidity and mortality. Quality improvement (QI) initiatives have successfully reduced post-operative hypothermia; however, maintaining these improvements presents a challenge due to the complex, multidisciplinary care required for surgical patients in the NICU. The benchmark set by U.S. News & World Report for optimal care is a hypothermia rate of less than 5%.
Objective: To sustain postoperative hypothermia rates below 5% in the NICU through December 2024.
Design/Methods: Since 2021, a multidisciplinary team composed of NICU, anesthesia, and surgery staff has been actively working to reduce post-operative hypothermia. Initial efforts lowered hypothermia rates from 14% (2021–2022) to 4% by the end of 2022, with sustained success throughout 2023 (Fig 1). However, in 2024, rates rose to 8.65%, particularly among infants with gestational age < 36 weeks or weight < 1500g, and those undergoing neurological or thoracic surgery. Key barriers identified included inconsistent use of isolettes, warming devices, temperature probes, and management of operating room (OR) temperatures.
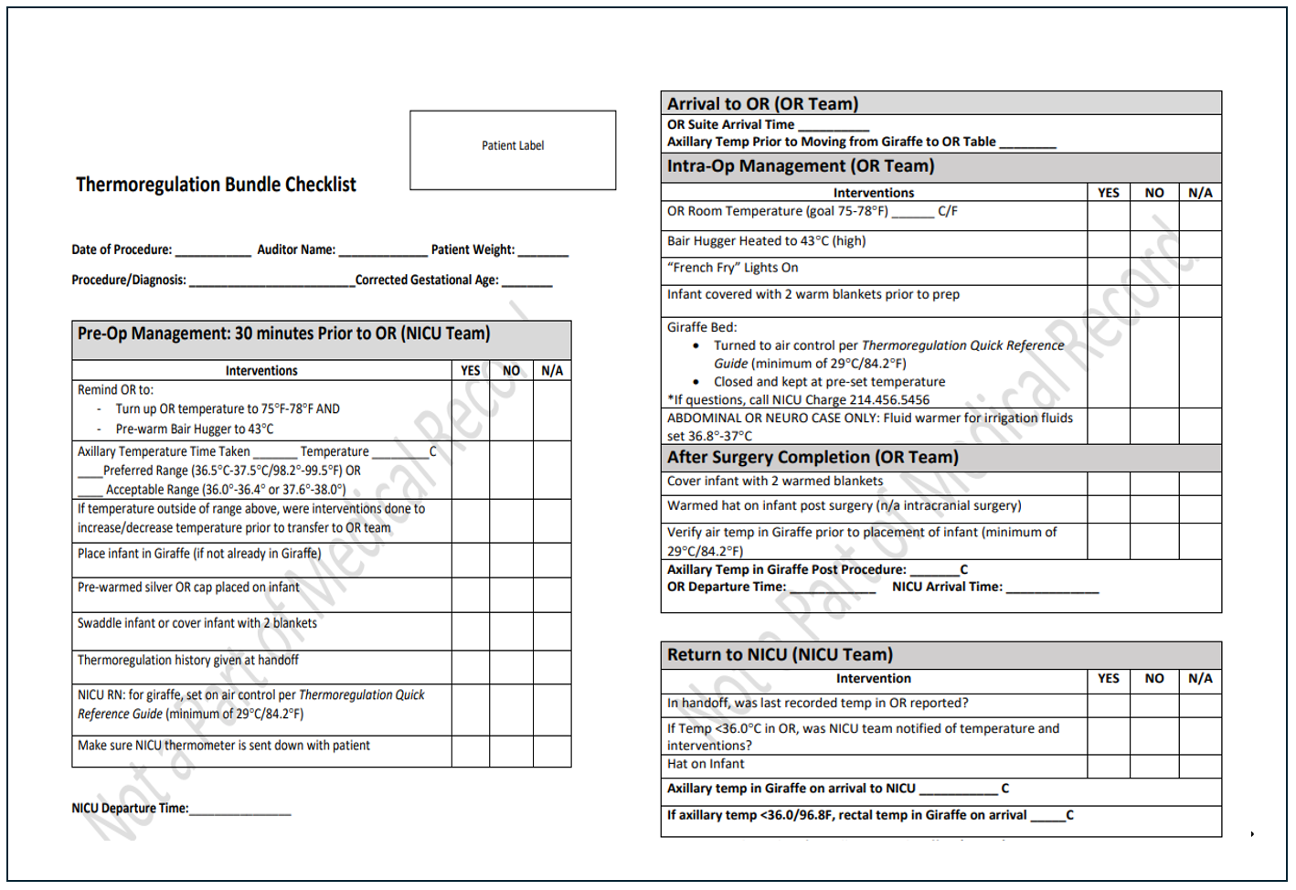
In response, the QI project was reinvigorated in 2024, implementing interventions focused on enhanced thermoregulation practices, checklist updates, and staff training (Fig 2). PDSA Cycle 1 included revisions to the bedside thermoregulation checklist (Fig 3), reinforcement of thermoregulation bundle protocols, and targeted training for OR staff on isolette use. PDSA Cycle 2 introduced further checklist enhancements and added warming of irrigation fluids for neurological and gastrointestinal procedures. Adherence to bundle components was monitored, with slight compliance improvements from 2023 to 2024. Going forward, root cause analysis of hypothermic cases will serve as a process measure to pinpoint opportunities for further improvement. Updates to the thermoregulation bundle are set to launch by the end of 2024.
Results: Hypothermia rates initially declined to 4% but subsequently increased to approximately 9% by mid-2024. While recent PDSA cycles showed intermittent improvements, achieving sustainable reductions remains a challenge.
Conclusion(s): Effective reduction of post-operative hypothermia in the NICU requires strong multidisciplinary collaboration. Although initial objectives were achieved, continued QI efforts and adaptive strategies are essential for long-term sustainability in maintaining normothermia for this vulnerable patient population
Figure 1. Hypothermic Patients Post Operative in the NICU with Interventions
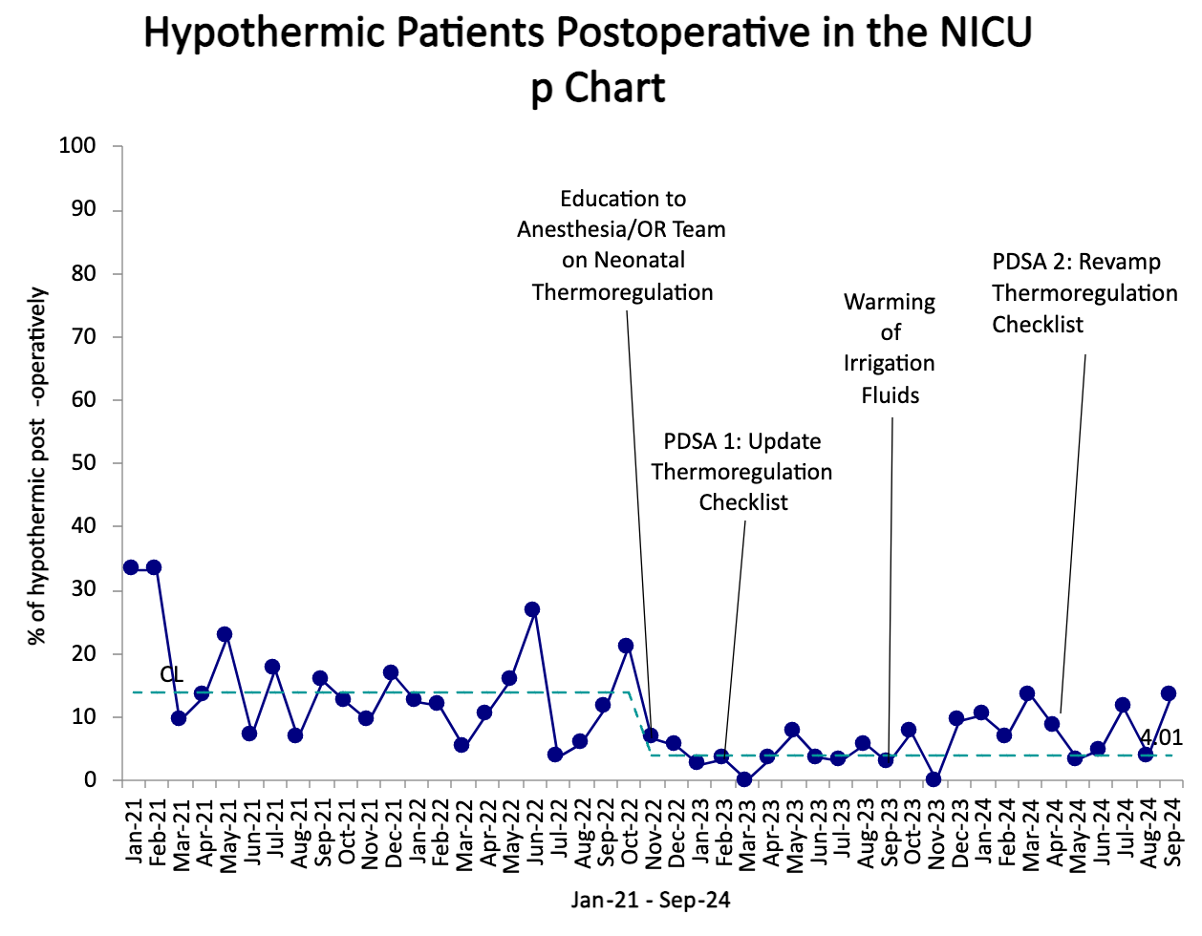
Figure 2. Key Driver Diagram
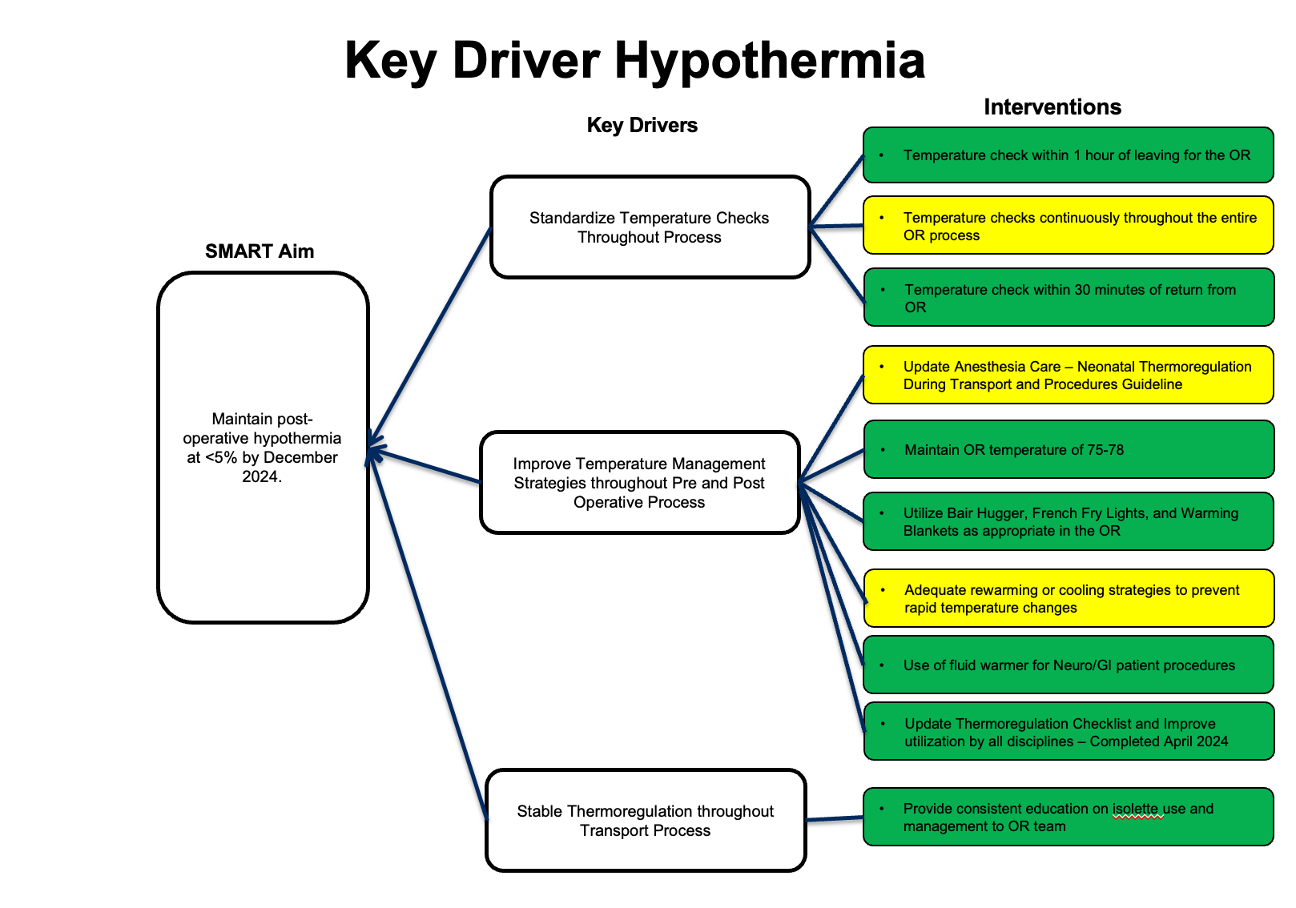
Figure 3: Thermoregulation Checklist