Technology 2: Telemedicine
Session: Technology 2: Telemedicine
190 - Increasing access to pediatric family-centered rounds for caregivers unable to be at bedside
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 190.5378
Tira Oskoui, University of California, Los Angeles David Geffen School of Medicine, Los Angeles, CA, United States; Esther Jun-Ihn, UCLA Mattel Childrens Hospital, Los Angeles, CA, United States; Kelly Fong, Seattle Children's, Seattle, WA, United States; Stacey Stauber, UCLA Mattel Childrens Hospital, Los Angeles, CA, United States; Kosuke Kawai, UCLA, Los Angeles, CA, United States; Yuliya Oumarbaeva-Malone, UCLA Mattel Childrens Hospital, Los Angeles, CA, United States; Helen Zhou, UCLA Mattel Childrens Hospital, Santa Monica, CA, United States; Amanda Kosack, UCLA Mattel Childrens Hospital, Los Angeles, CA, United States; Jessica Lloyd, UCLA, Los Angeles, CA, United States
Helen Zhou, MD (she/her/hers)
Assistant Clinical Professor
UCLA Mattel Childrens Hospital
Santa Monica, California, United States
Presenting Author(s)
Background: There are many advantages of family-centered rounds (FCR). However, FCR is not readily accessible to caregivers who cannot remain physically present at bedside. After utilizing secure virtual FCR during the COVID-19 pandemic, this study explores caregiver perspectives on the feasibility and utility of providing virtual FCR beyond the pandemic.
Objective: Describe caregivers’ barriers to being physically present at FCR and identify potential strategies to improve access to FCR.
Design/Methods: We designed a prospective mixed-method study for patient caregivers admitted to a quaternary academic center, including questions about participation in FCR, language concordance, internet access, demographics, and interest in a virtual option for FCR. The rounding medical team identified participants for a 6-month enrollment period. Caregivers were recruited in person or via phone and answered questions in their preferred language. We used descriptive statistics for close-ended questions and thematic analysis for open responses. Fischer exact test for categorical variables and Wilcoxon rank sum test for continuous variables were utilized to compare respondents’ characteristics by frequency of participation in FCR, primary spoken language and demographics.
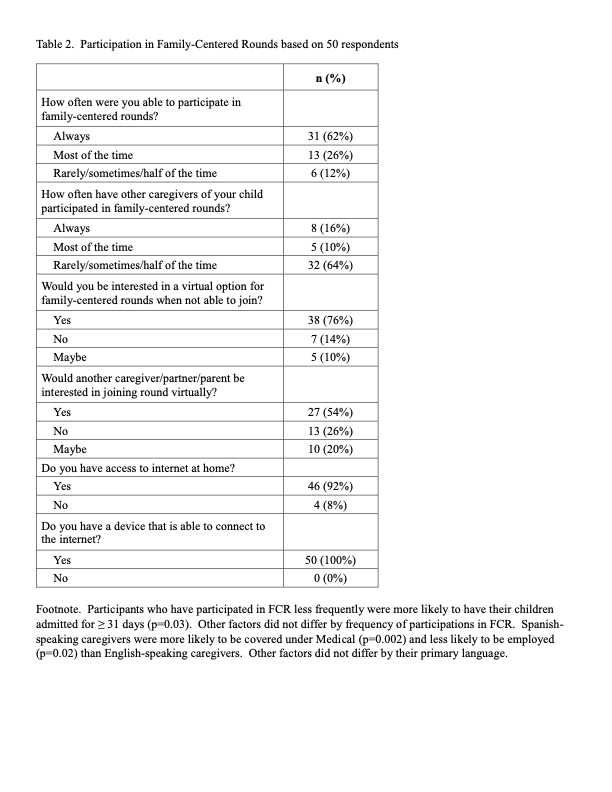
Results: 50 caregivers completed the survey; 38% were absent during FCR. Most self-identified as Hispanic or Latino (54%), 22% of participants primarily spoke Spanish and 60% utilized public insurance (Table 1). Barriers to being at the bedside included childcare, work, and transportation, respectively (Table 2). 76% of caregivers were interested in a virtual option for FCR and 54% stated other caregivers might also be interested in joining if there was a virtual FCR (Table 2). Interest in virtual FCR did not differ by sociodemographic factors. Suggestions to increase engagement in FCR included scheduling rounds at a set time, standardizing the process for providing phone updates, and including caregiver communication preference during staff handoffs.
Conclusion(s): This is one of the first studies to explore the experiences of caregivers who are not at the bedside and includes caregivers who speak a primary language other than English. Our findings highlight FCR barriers families face and demonstrates high interest in a virtual FCR option. Potential FCR-supportive interventions include offering a virtual option for rounds and increasing resources such as transportation reimbursement. Future work includes creating a new inpatient FCR interface, additional training for medical team and standardizing communication practices with caregivers.
Table 1. Baseline characteristics of 50 participants
.png)
Table 2. Participation in Family-Centered Rounds based on 50 respondents