Emergency Medicine 4
Session: Emergency Medicine 4
248 - Increasing Referrals to Substance Use Navigation for Adolescents With Substance Use Disorder
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 248.5337
Michele McDaniel, University of California, San Diego School of Medicine, San Diego, CA, United States; Russell Gagui, Rady Children's Hospital San Diego, San Diego, CA, United States; Erin Dale, Rady Children's Hospital San Diego, San Diego, CA, United States; Hannah Perkins, Rady Children's Hospital San Diego, San Diego, CA, United States; Monica Felix, Rady Children's Hospital San Diego, San Diego, CA, United States; Shelley Sherman, Rady Children's Hospital San Diego, San Diego, CA, United States; Monica Angeles, Rady Children's Hospital San Diego, Escondido, CA, United States; Rachel Stengone, Rady Children's Hospital San Diego, San Diego, CA, United States; Amy Bryl, Rady Children's Hospital/University of California San Diego, San Diego, CA, United States

Michele McDaniel, MD (she/her/hers)
HS Clinical Associate Professor of Pediatrics
University of California, San Diego School of Medicine
SAN DIEGO, California, United States
Presenting Author(s)
Background: Entrance of youth with substance use disorder (SUD) into treatment programs decreases substance use. Prescription of buprenorphine/naloxone to youth with opioid use disorder (OUD) increases their retention in treatment.
Objective: Our QI initiative aimed to increase the percent of pediatric emergency department (ED) visits with a high-risk CRAFFT screen or substance use disorder diagnosis referred to a substance use navigation (SUN) program from 0 to 50% in 12 months and to prescribe buprenorphine/naloxone in all ED visits with an OUD diagnosis that were discharged from the ED.
Design/Methods: A multidisciplinary team of ED physicians, nurses, social workers, pharmacists, and a substance use navigator developed a process to identify, treat, refer, and connect patients with SUDs. We constructed a key driver diagram (Figure 1). Key interventions included physician education on SUD identification and OUD treatment, embedding a SUN referral order into physician and SW electronic medical record workflows, and enabling the prescription and dispensation of buprenorphine/naloxone from our pharmacy. Additional measures included the percent of referred patients who were successfully contacted, the percent of patients contacted who were connected to treatment, and the percent of return visits with a SUD diagnosis. We used statistical process control to examine changes in measures over time.
Results: From March 2023 to August 2024, we increased the percentage of at-risk ED visits referred to SUN from 0 to 34% (Figure 2). Buprenorphine/naloxone was prescribed in 75% (3/4) of visits with OUD discharged from the ED; in the visit where the drug was not prescribed, the patient was connected to outpatient MAT services by SUN. There were no prescriptions for buprenorphine/naloxone in ED visits with an OUD diagnosis that were admitted to inpatient medical or psychiatric services (0/5). Of patients referred to SUN, 60% (83/138) were successfully contacted, 46% (38/83) of those contacted were connected to substance use treatment, and 39/83 (47%) of those contacted were connected to behavioral health support. The percent of ED visits with a SUD diagnosis that were a re-visit remained at 12%.
Conclusion(s): We increased the percentage of at-risk ED patients referred to a SUN program from 0 to 34%, prescribed buprenorphine/naloxone in ED visits with OUD, and connected patients to treatment. Next steps will focus on continued education and hardwiring of these processes as well as spreading this work to the inpatient psychiatric and medical settings.
Figure 1
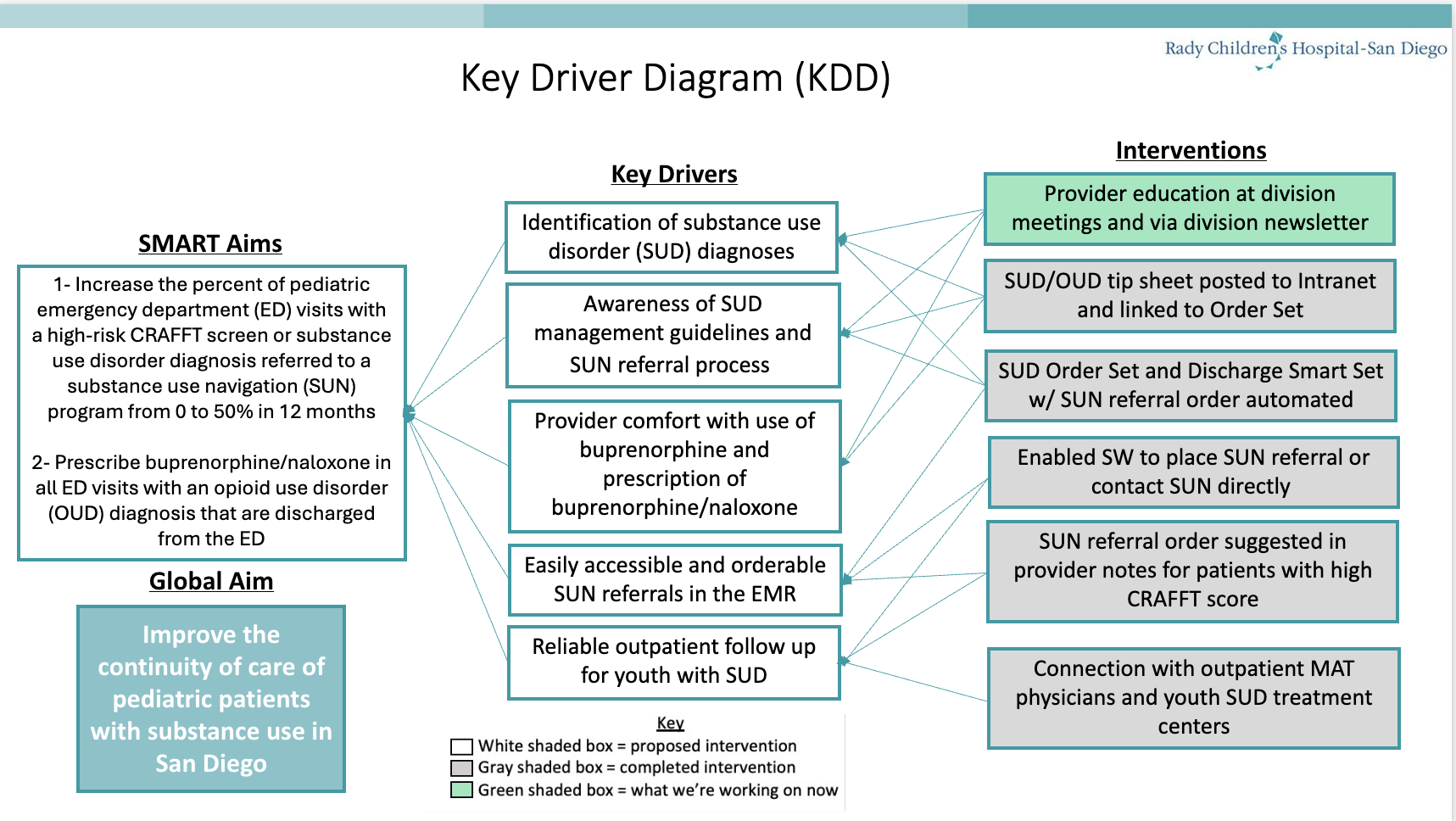 Key Driver Diagram
Key Driver DiagramFigure 2
.png) Control Chart
Control Chart

