Neonatal Nephrology/AKI 2
Session: Neonatal Nephrology/AKI 2
023 - Incidence and Outcomes of Neonatal Acute Kidney Injury: A Multicentre Observational Cohort Study in Australia and New Zealand (NeoKANZ)
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 23.5317
Eveline Staub, Royal North Shore Hospital, St Leonards, New South Wales, Australia; Amanda Dyson, The Canberra Hospital, canberra, Australian Capital Territory, Australia; Tim Schindler, Royal Hospital for Women, Sydney, New South Wales, Australia; Sunaina Nundeekasen, The Canberra Hospital, canberra, Australian Capital Territory, Australia; Angelica Allermo Fletcher, Wellington Regional Hospital, Wellington, Wellington, New Zealand; Helen G. Liley, The University of Queensland, South Brisbane, Queensland, Australia; Alison L. Kent, University of Rochester, NY, USA, Henley Beach, South Australia, Australia

Eveline Staub, MD MMed FRACP CCPU (she/her/hers)
Unit Director and Staff neonatologist
Royal North Shore Hospital
St Leonards, New South Wales, Australia
Presenting Author(s)
Background: Neonatal acute kidney injury (AKI) is associated with adverse short- and long-term outcomes including increased risk of mortality, morbidity during NICU admission and increased risk of developing chronic kidney disease. AKI has been shown to be prevalent in neonatal populations outside Australia and New Zealand (ANZ), but the incidence in ANZ neonatal intensive care units (NICU) is not known.
Objective: The aim of this study is to assess the incidence of neonatal AKI in the ANZ NICU setting.
Design/Methods: Retrospective chart review of all neonates admitted < 14 days of age to 5 perinatal and surgical NICUs in Australia and New Zealand from 1/1/2019 to 30/6/2019. Exclusion criteria included: death < 48hrs of life, intravenous fluid therapy < 48 hrs, severe congenital kidney or urinary tract abnormalities, lethal chromosomal anomalies, congenital heart disease requiring surgical repair or prostaglandin infusion in the first week of life. Data were collected on demographics, morbidity and mortality and kidney function during NICU admission. We defined AKI using modified KDIGO criteria (increase in serum creatinine ≥ 27umol/l or > 50% from previous lowest value, or urinary output of < 1ml/kg/hour).
Results: 794 neonates were included (median gestational age 34.1 weeks (range 23.0-42.1), median birth weight 2090g (range 420-5070). Of these, 600 (75.6%) of included neonates (characteristics shown in table 1) had sufficient data to ascertain AKI status, with available data varying between the 5 centres from 53.5% to 95.7% of total included neonates. 150 infants (25.0%) had at least one episode of AKI documented of which 65.2% were identified by serum creatinine criteria alone, 16.0% by urine output criteria alone, and 34.8% by both criteria. AKI incidence varied by gestational age group: 25.6% of infants born < 29 weeks had an episode of AKI, 19.9% in the group born 29-35 weeks, 32.8% in neonates ≥36 weeks (figure 1). Overall, mortality was similar in both groups: AKI 6.0% vs. no AKI 3.6% (p=0.24), as was median length of stay (AKI 31.3 days (range 1 -168) vs. no AKI 29.6 days (1-153), p=0.65)
Conclusion(s): Neonatal AKI is common in neonates admitted to ANZ NICUs, with the highest incidence in the group of neonates ≥36 weeks’ gestation. Incidence of AKI is likely underreported because assessment of renal function in neonates admitted to NICUs varies across different centres.
Table 1. Basic characteristics according to three gestational age groups for infants with sufficient data to ascertain AKI status.
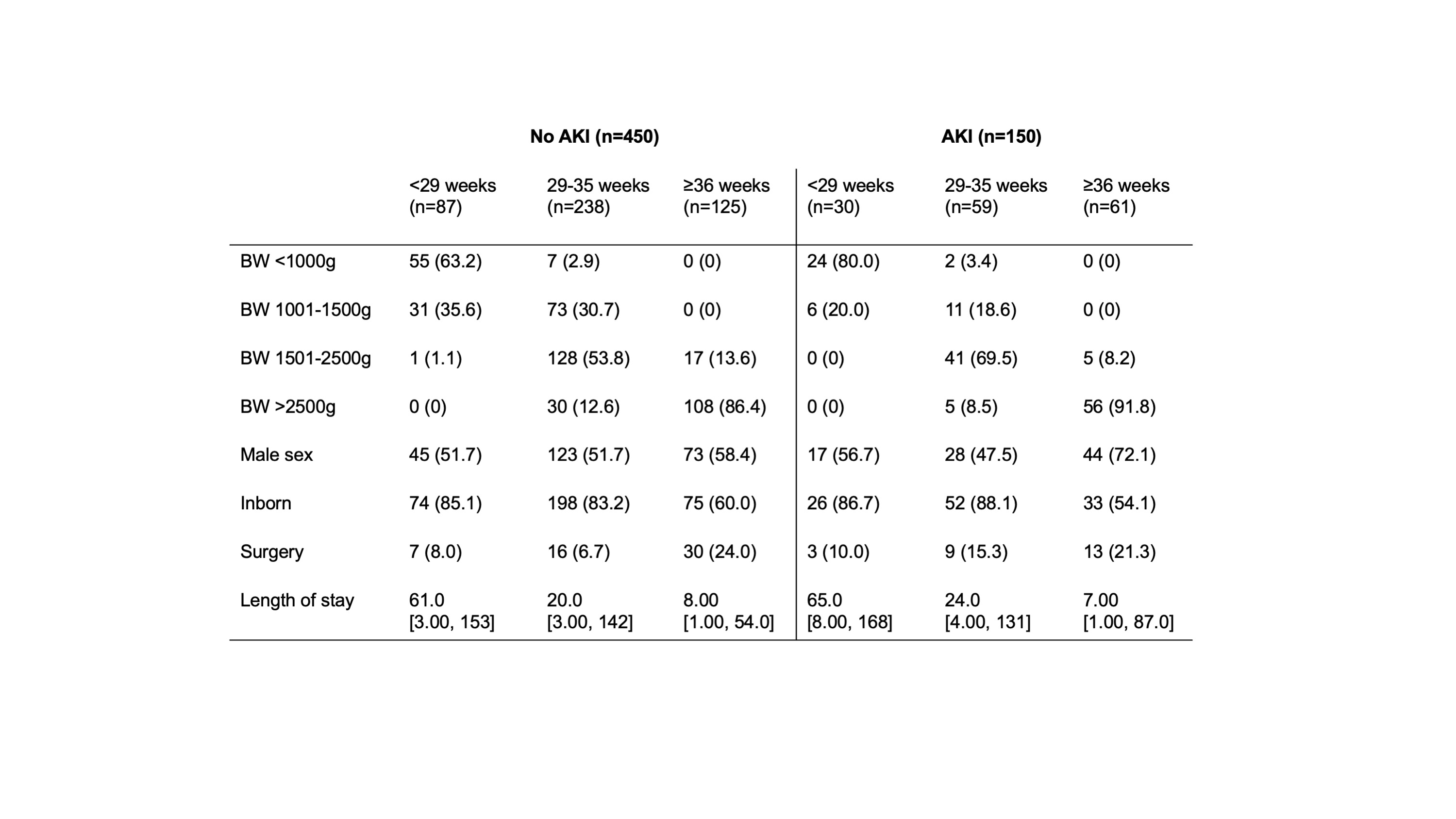 BW: birth weight. Numbers are n with percent in brackets, or median with range in brackets.
BW: birth weight. Numbers are n with percent in brackets, or median with range in brackets.Figure 1.
Figure 1.jpegAbsolute numbers and proportions of infants in three gestational age groups ( <29 weeks, 29-35 weeks, 36 weeks) with and without acute kidney injury (AKI) (of the 600 study participants with sufficient data to ascertain AKI status).

