Neonatal Quality Improvement 6
Session: Neonatal Quality Improvement 6
538 - Limiting Intervention, Improving Outcomes, and Reducing Length of Stay for Infants with Transient Tachypnea of the Newborn in the Neonatal Intensive Care Unit
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 538.5882
Sushma Krishna, Icahn School of Medicine at Mount Sinai, Harrington Park, NJ, United States; Richelle Reinhart, Icahn School of Medicine at Mount Sinai, New York, NY, United States; Malorie Meshkati, The Mount Sinai Kravis Children's Hospital, New York, NY, United States; Sarah Bennett, Mount Sinai Health System, New York, NY, United States; Brittany Smith, The Mount Sinai Kravis Children's Hospital, New York, NY, United States; Courtney Juliano, Icahn School of Medicine at Mount Sinai, New York, NY, United States
- SK
Sushma Krishna, MD (she/her/hers)
Neonatologist
Icahn School of Medicine at Mount Sinai
Harrington Park, New Jersey, United States
Presenting Author(s)
Background: Transient Tachypnea of the Newborn (TTN) is a common neonatal respiratory disorder. Affected infants may require admission to the neonatal intensive care unit (NICU), respiratory support, and other interventions such as intravenous (IV) catheter placement and fluid administration.
Objective: To improve outcomes for infants with TTN by standardizing care, minimizing unnecessary intervention, and reducing length of stay (LOS). Our smart aim was to reduce NICU LOS in neonates ≥ 35 weeks admitted with TTN by 15% by December 2024.
Design/Methods: This quality improvement (QI) project was conducted using the model for improvement. We developed a smart aim, created a key driver diagram, and implemented serial interventions across two NICU sites (Level III and IV). These included TTN management guideline development, weekly case audits, roll-out of nurse-driven respiratory weaning, and creation of an electronic medical record (EMR) order-set.
Data was collected retrospectively from January 2023-May 2024 and prospectively from June 2024. The primary outcome measure was LOS. Additional outcome measures included time to first feed, time on respiratory support, and incidence of hyponatremia, IV placement, and IV fluid administration. Balancing measures were readmissions, occurrence of hypoglycemia, and exposure to formula feeding.
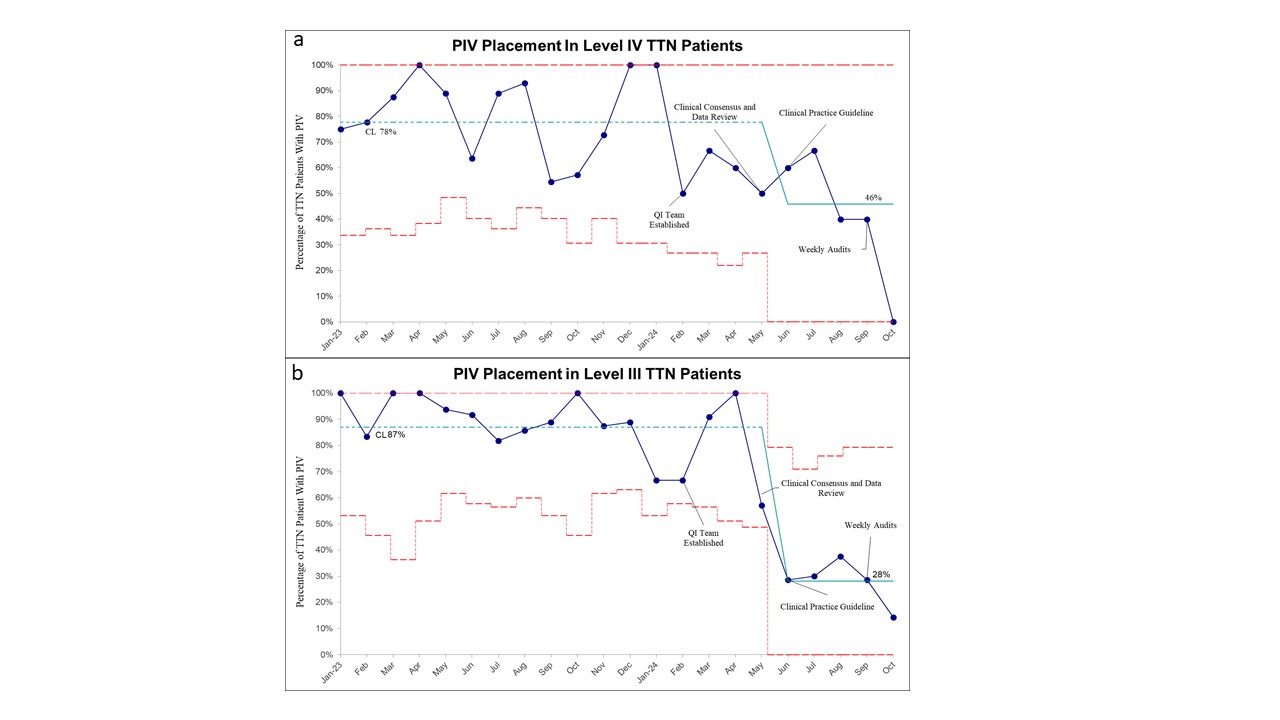
Results: NICU LOS decreased from 83h to 46h (Level IV) and 66h to 49h (Level III). Time to first feed downtrended (Level IV) and decreased from 565m to 167m (Level III). Time on respiratory support decreased from 26h to 16h (Level IV) and 26h to 14h (Level III). Hyponatremia decreased from 36% to 13% (Level IV) and 46% to 5% (Level III). IV fluid administration decreased from 77% to 42% (Level IV) and 85% to 26% (Level III). IV placement decreased from 78% to 46% (Level IV) and 87% to 28% (Level III). There was no increase in readmissions or hypoglycemia. Formula feeding increased from 90% to 100% (Level III).
Conclusion(s): This QI initiative, which prioritized standardization of care via guideline development, case audits, and use of an EMR order set, led to shorter time on respiratory support, reduced time to first enteral feed, lower rates of PIV placement and IVF administration, and an overall shorter LOS for infants with TTN in both NICUs. The Level III NICU had a modest increase in number of infants receiving formula feeding. Future interventions may include EMR respiratory assessment scoring to improve nurse driven respiratory weaning and use of donor breast milk to limit exposure to formula.
Figure 1. Annotated X-Bar chart (with accompanying S-chart) showing length of stay for infants with TTN at level IV (a) and level III (b) NICU sites
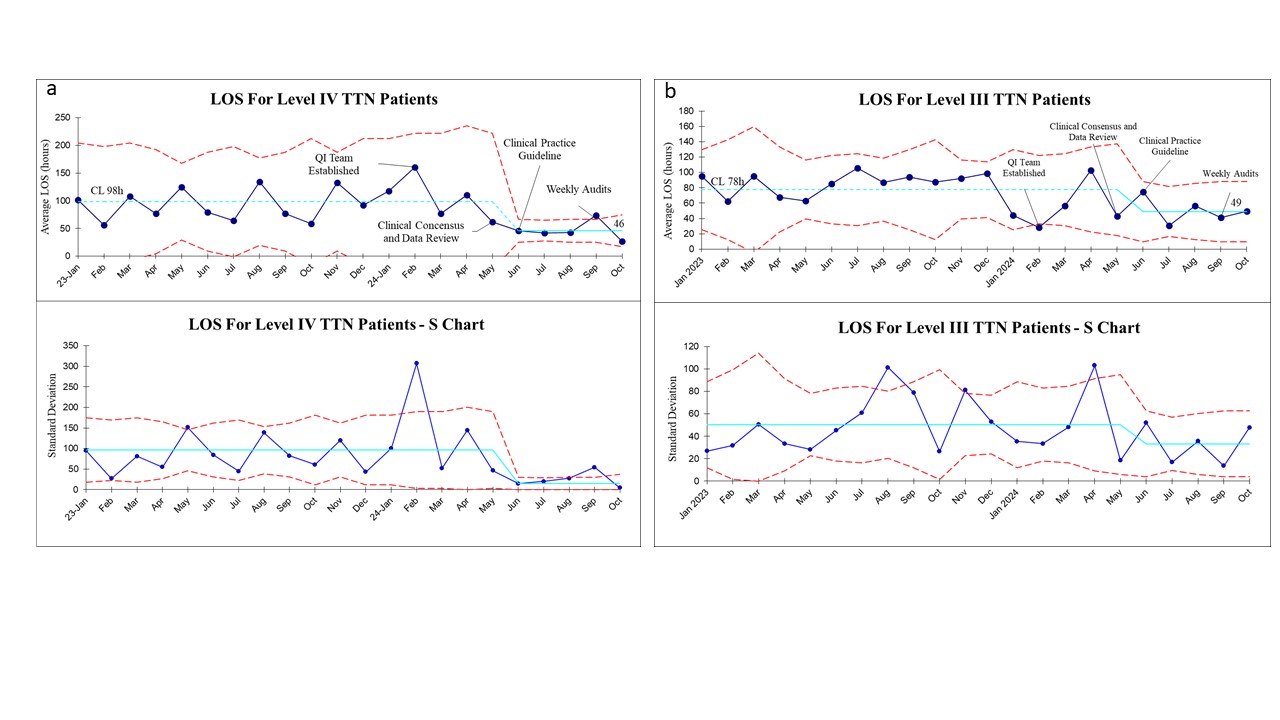
Figure 2. Annotated X-Bar chart (with XbarS-chart) showing duration of CPAP for infants with TTN at level IV (a) and level III (b) NICU sites.
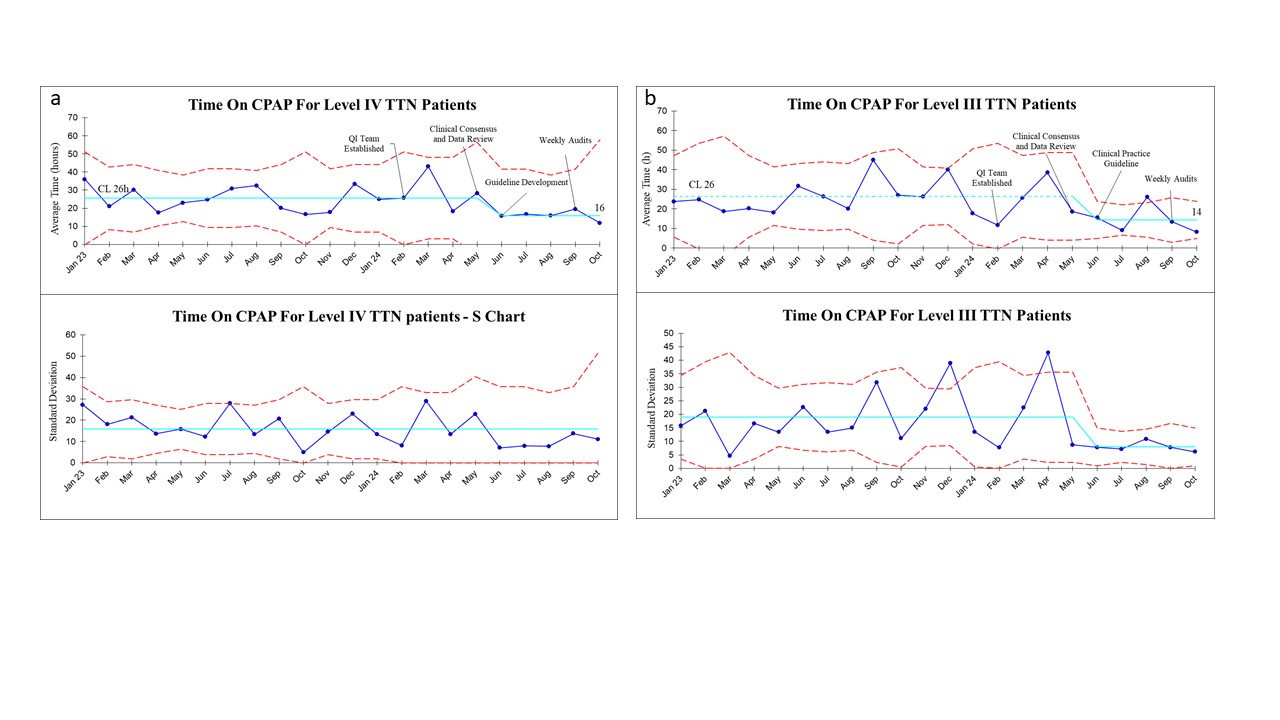
Figure 3. Annotated p-chart showing percentage of patients with TTN who had PIV placed at level IV (a) and level III (b) NICU sites.