Mental Health 1
Session: Mental Health 1
754 - Comparison of practices’ consults to a pediatric mental health care access program: Initial vs subsequent consults.
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 754.4490
Jeanne Van Cleave, University of Colorado School of Medicine, Aurora, CO, United States; Susan E. Young, University of Colorado, Longmont, CO, United States; Ryan Asherin, University of Colorado Anschutz, Littleton, CO, United States; David M. Keller, Children's Hospital Colorado, Aurora, CO, United States; Kaitlin Whelan, University of Colorado School of Medicine, Golden, CO, United States; sandra Fritsch, University of Colorado School of Medicine, Aurora, CO, United States
- JV
Jeanne Van Cleave, MD (she/her/hers)
Associate Professor
University of Colorado School of Medicine
Aurora, Colorado, United States
Presenting Author(s)
Background: Pediatric mental health care access programs (PMHCAs) are state- or regional-level programs that offer primary care clinicians (PCPs) timely consultation and referral assistance from child mental health clinicians for patients with mental health conditions. Consults are conducted by telephone or asynchronous e-platform. As these programs mature, understanding how consults from primary care practices evolve over time can guide modifications in the PMHCAs’ educational programming and outreach to PCPs.
Objective: We aimed to compare practices’ initial consults with subsequent consults, with a focus on consult outcome, clinical severity and complexity.
Design/Methods: We analyzed data from consults completed by Colorado's PMHCA between Sept 2019-May 2024. Consults were identified as a practice's initial consult or second through twentieth consults. We compared elements of consults, including types of questions, content discussed, outcomes, diagnoses, clinical severity, and consult complexity, and length of phone call, between initial and subsequent consults using multivariate techniques, adjusting for patient age, gender and insurance.
Results: There were 257 initial consults and 1225 subsequent consults. Compared to initial consults, subsequent consults were more likely to be for ongoing medication management (56% vs 42%, p< 0.001, AOR 1.7, 95% CI 1.2-2.3), include medication changes (59% vs 50%, p=0.008; AOR 1.4, 95% CI 1.0-1.8), and include a recommendation for psychotherapy (38% vs 32%, p=0.04; AOR 1.5, 95% CI 1.1-2.0). Patients who were the subject of subsequent consults were more likely to have management of their mental health conditions remain within primary care versus referral to psychiatry (56% vs 47%, p=0.006; AOR 1.4, 95% CI 1.1-1.9). However, subsequent consults and initial consults did not differ in clinical severity, number of medication classes discussed, length of call, or type or total number of diagnoses discussed.
Conclusion(s): Compared to a practice's initial consult, subsequent consults to a PMHCA differed in recommendations discussed, had a greater focus on medication management, and were more likely to result in care remaining in primary care. However, subsequent consults were not more complex or for more impaired patients. It appears that with continued use of the PMHCA, PCPs are expanding their capacity to be the primary manager of patients with mild-moderate mental health conditions, particularly in regard to medication management.
Table 1. Characteristics of patients who prompted practices’ initial versus subsequent consults.
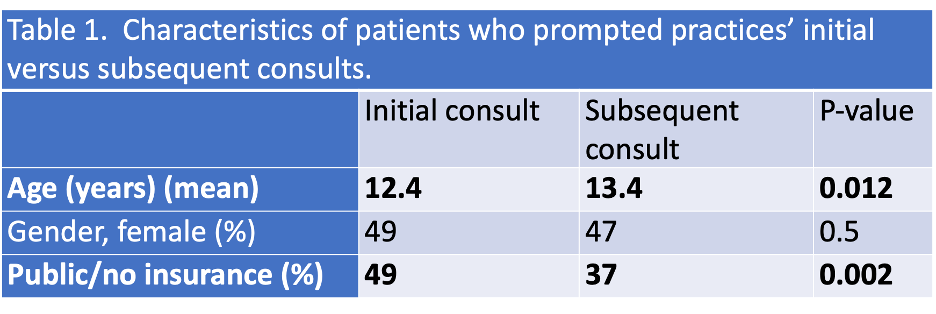
Table 2. Association between subsequent consult status and content, severity and complexity of the consult.
.png)

