Emergency Medicine 6
Session: Emergency Medicine 6
278 - Effectiveness of a Clinical Pathway on Reducing Antibiotic Duration for Community Acquired Pneumonia in Pediatric Urgent Care Clinics
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 278.4763
Marsha Dannenberg, Children's Mercy Hospitals and Clinics, Overland Park, KS, United States; Todd Glenski, Children's Mercy Kansas City, Kansas City, MO, United States; Joshua A. Saucedo, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Rana E. El Feghaly, Children's, Kansas City, MO, United States; Brian R. Lee, Children's Mercy Hospital, Kansas City, MO, United States; Leslie Ann. Hueschen, Children's Mercy Hospital/ University of Missouri-Kansas City, Kansas City, MO, United States; Amanda Nedved, Children's Mercy Hospitals and Clinics, Lenexa, KS, United States

Marsha Dannenberg, MD
Assistant Professor of Pediatrics
Children's Mercy Hospitals and Clinics
Overland Park, Kansas, United States
Presenting Author(s)
Background: Prolonged antibiotic treatment durations can increase the risk of adverse effects, healthcare costs, and antibiotic resistance. Recent studies suggest 3-5 day antibiotic treatment courses for uncomplicated community acquired pneumonia (CAP) are safe and effective. Since Urgent Care (UC) clinicians frequently encounter and treat respiratory illnesses such as CAP with antibiotics, they are an important target for antibiotic stewardship initiatives that decrease treatment durations.
Objective: To evaluate the effectiveness of a clinical pathway (CP) and order set on shortening durations of antibiotics for children diagnosed with uncomplicated CAP in 3 UC clinics.
Design/Methods: A multidisciplinary team developed a CP based on published evidence-based medicine (Figure 1) which recommended 3-5 days of antibiotic therapy for uncomplicated CAP (Table 1). The implementation strategy included initial review of the CP by UC clinicians in January 2024, followed by publication of the CP online in March 2024 alongside an electronic order set with pre-completed prescriptions defaulted to 3- and 5-days duration. We reviewed encounters of all patients discharged with uncomplicated CAP in 3 UC clinics during the baseline (March-December 2023) and post-implementation period (March-September 2024). We considered January-February 2024 a washout period. We excluded encounters that either had no antibiotic or azithromycin prescribed. We measured the percentage of antibiotics prescribed for ≤ 5 days as our primary outcome and used Pearson’s Chi-square test to compare differences between the 2 time periods. We also trended the percent over time and calculated the potential days of therapy (DOT) avoided based on shorter prescribing practices.
Results: We reviewed 527 encounters (baseline) and 930 encounters (post-intervention). Following implementation of the CP in March 2024, we saw an increase in the percent of antibiotic duration of ≤ 5 days from 6.6% to 22.3% (p < 0.001). The initial increase coincided with circulation of the CP to UC physicians in January 2024. The increase has been sustained (Figure 2). We potentially avoided 414 DOT for antibiotics in the post-implementation period compared to 70 in the pre-implementation period.
Conclusion(s): Our results indicate that implementing an organizational CP and order set can successfully promote shorter durations of antibiotics for uncomplicated CAP in UC clinics. Future steps include using quality improvement methodology to develop future interventions with balancing measures to monitor treatment failures.
Figure 1
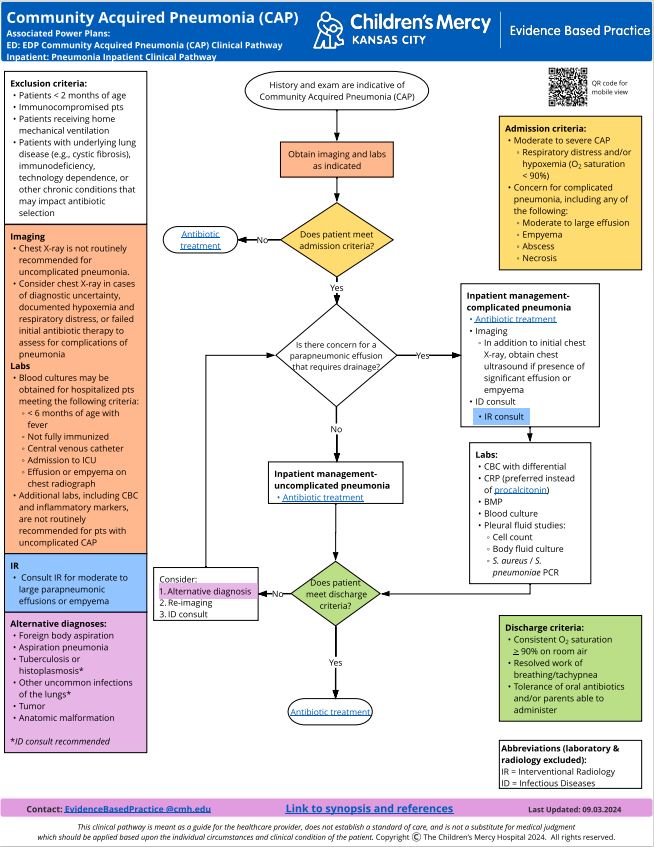 Our institution's clinical pathway for community acquired pneumonia
Our institution's clinical pathway for community acquired pneumoniaTable 1
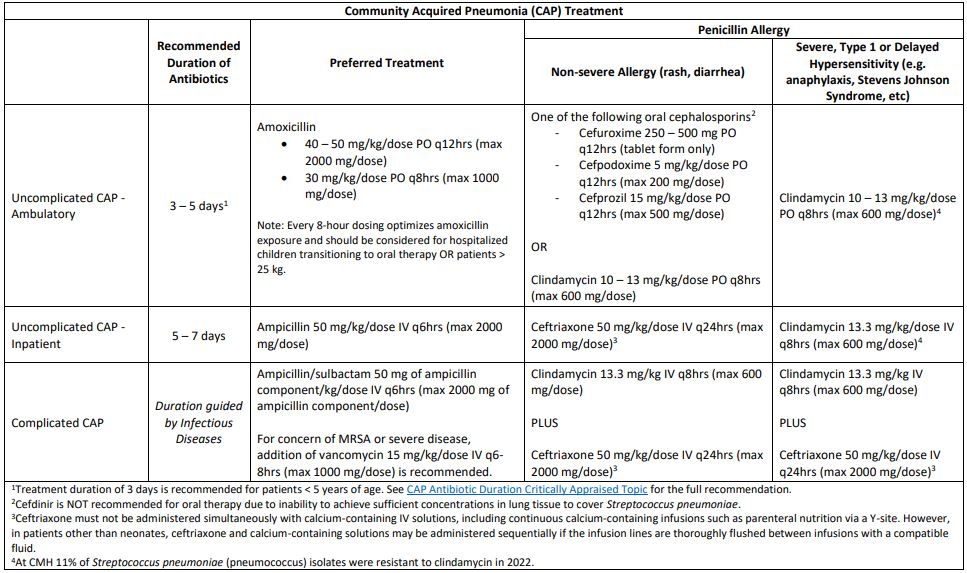 Recommended antibiotic durations for community acquired pneumonia
Recommended antibiotic durations for community acquired pneumoniaFigure 2
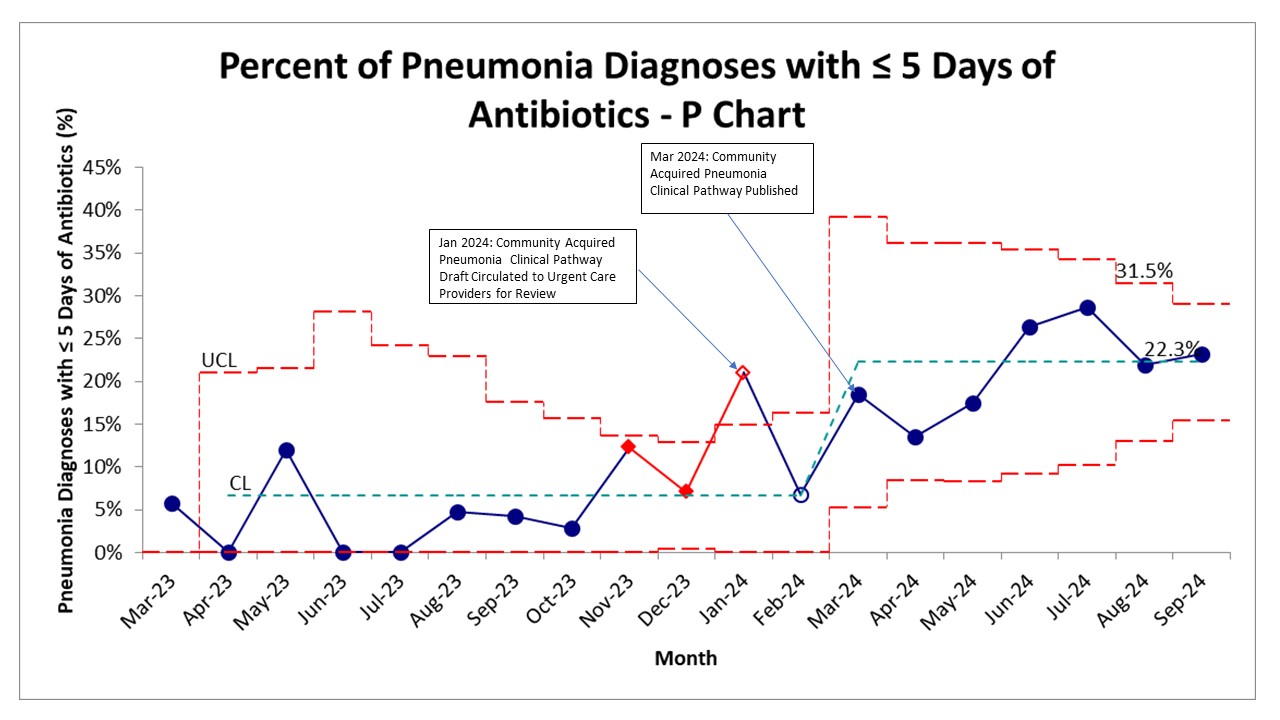 P chart of percent of community acquired pneumonia with antibiotic duration of 5 days or less over time.
P chart of percent of community acquired pneumonia with antibiotic duration of 5 days or less over time.

