Clinical Bioethics
Session: Clinical Bioethics
573 - Addressing Bias, Power, and Oppression in Pediatric Bioethics Consultation
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 573.3957
Brian S.. Carter, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Sarah Porter, Randall Children's Hospital at Legacy Emanuel, Portland, OR, United States

Sarah Porter, MSW, LCSW (she/her/hers)
Manager - Social Work, Clinical Ethics Consultant
Randall Children's Hospital at Legacy Emanuel
Portland, Oregon, United States
Presenting Author(s)
Background: In pediatric bioethics clinical consultation, there is often a lack of consideration of the roles of bias, power, and oppression in conducting pediatric bioethics consultation and determining the most effective recommendation for the clinical team, family, or patient. While these topics have been ever-present, they are complex and not typically situated in common bioethical analyses. With increasing attention to the social determinants of health, diversity, equity, and inclusion, attending to both personal and social justice in a meaningful manner is needed.
Objective: Present a model for integrating attention to bias, power, and oppression within a commonly used approach to pediatric bioethics clinical consultation and generating potential solutions to difficult clinical ethics matters.
Design/Methods: We present a pediatric bioethics clinical consultation case involving a 1-year-old medically complex child with significant psychosocial challenges to illuminate how bias, power, and oppression can be addressed by taking an “ethical pause and reflection” at different stages of the case analysis. The accompanying figure illustrates how an intentional pause with reflection and deliberation attends to these matters (see Figure).
Results: This case illustrates how reframing a pediatric bioethics clinical consultation case analysis using an intentional process of reflection can encourage the ethics consultant to check for power imbalance between the clinical team and the patient/family. It also reveals how a reflective process can lead to evaluating decisions and alternatives to mitigate the negative impact(s) of clinician, consultant, and family perceptions of bias, power, and oppression, and both consider and incorporate cultural factors in the final recommendation.
Conclusion(s): This new model for PBC case analysis presents a useful tool that should be evaluated in future trials to assess its utility.
Figure
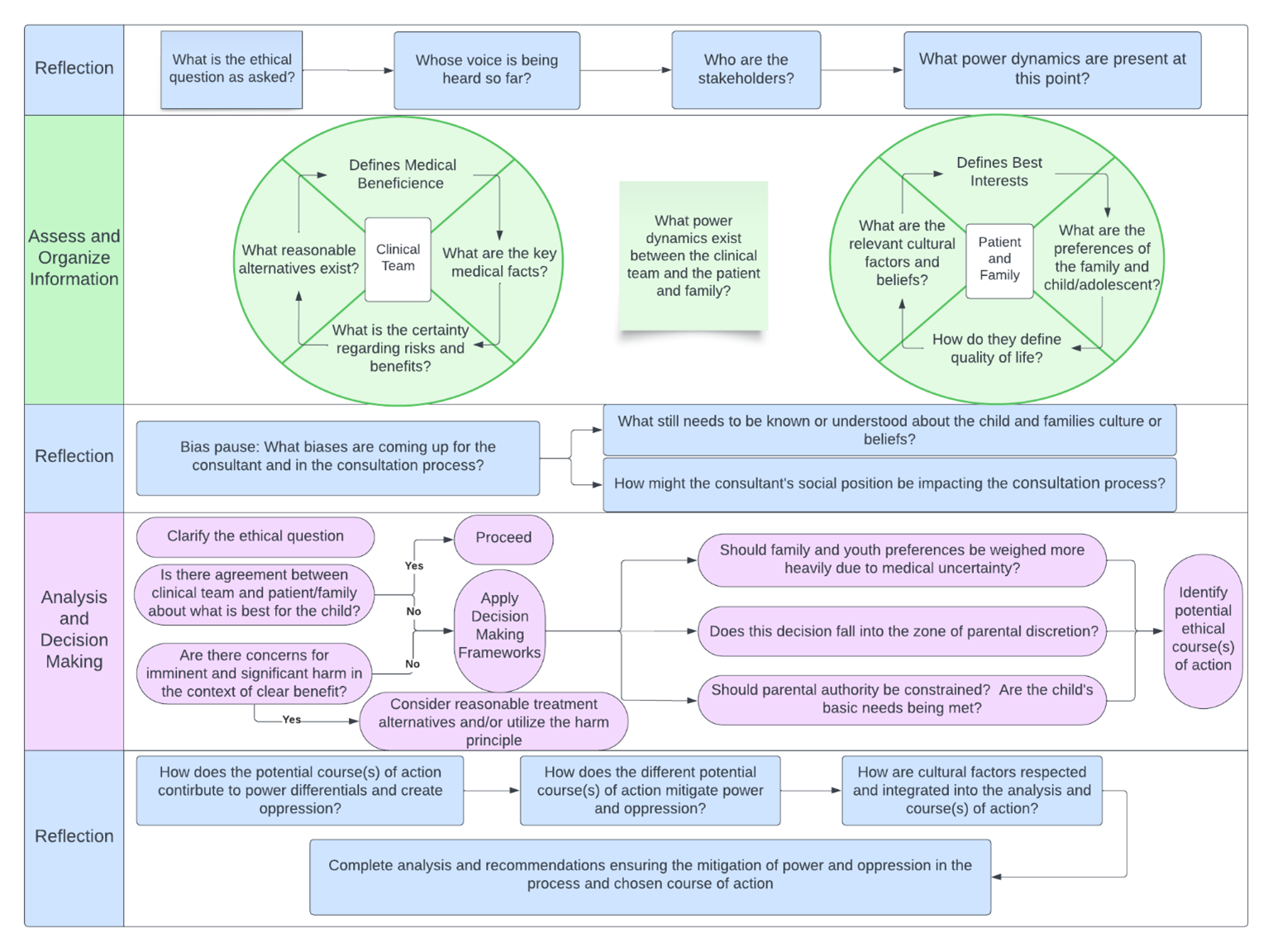 Insertion of an "Ethical Pause and Reflection" into a pediatric bioethics consultation case analysis to mitigate bias, power, and oppression in deriving an ultimate recommendation.
Insertion of an "Ethical Pause and Reflection" into a pediatric bioethics consultation case analysis to mitigate bias, power, and oppression in deriving an ultimate recommendation.
