Emergency Medicine 5
Session: Emergency Medicine 5
262 - Disparities in the Emergency Evaluation and Management of Unintentional Ingestions in Preschool Children
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 262.4060
Jennifer Allen, Akron Children's Hospital, Akron, OH, United States; Charles Foust, Akron Children's Hospital, Shaker Heights, OH, United States; Michelle Bestic, Akron Children's Hospital, Hudson, OH, United States; Neil L. McNinch, Akron Children's Hospital, Kent, OH, United States; Michael L. Forbes, Northeast Ohio Medical University, Akron, OH, United States

Jennifer Allen, DO
Pediatric Emergency Medicine Fellow
Akron Children's Hospital
Akron, Ohio, United States
Presenting Author(s)
Background: Unintentional injuries consisting of trauma and poisonings are the leading cause of death in patients aged 1-4 years old with a significant portion attributed to ingestions. National Poison Control data in 2021 showed there were 37 incidences of poison exposure per 1000 children under 6 years old (2023). Between 2010-2019, poisoning deaths among minority children increased (West, 2021). Evidence of treatment disparity exists as seen in the decreased use of opioids or analgesia in minority children with long bone fractures or appendicitis in the emergency department (ED) (Goyal, 2015 and 2020). There is a knowledge gap regarding the extent, causes, and impact of disparities in assessing and managing acute ingestions in children.
Objective: This study aimed to determine whether there is a difference in the evaluation and management of children with unintentional ingestions in a pediatric tertiary care center’s ED.
Design/Methods: From January 2013 to March 2024, patients less than 6 years of age were identified by International Classification of Disease (ICD) 9 and 10 codes in the electronic health record (EHR). Independent variables included: race, childhood opportunity index (COI), payor status, severity, age, sex, and substance type. Dependent variables included: urine drug screen (UDS), social work (SW) consult, and child service bureau (CSB) referral. Summary statistics were calculated and described as mean (sd). The relationship between independent and dependent variables was described using odds ratio (OR) with 95% confidence interval (CI). The relationship between pharmaceutical ingestion type was described using the receiver operating characteristic curve (ROC). Significance was defined as p-value < 0.05. Races are defined as White, African American, and Other.
Results: 4411 patients had unintentional ingestions, and most ingestions were non-pharmaceutical (56%). Patients with pharmaceutical ingestions had higher odds of a social work consult and a CSB referral (OR 8.3, 9.0). Private insurance and ED discharge were associated with reduced odds of SW consults or CSB referral. A lower COI was associated with higher odds of SW consult and CSB referral (Table 1). When adjusted for COI, payor type, and severity, African Americans had higher odds of a SW consult, CSB referral, and UDS order (OR 1.8, 2.8, 2.3).
Conclusion(s): This study revealed there are racial disparities in the management of unintentional ingestions within the ED setting. The next step would be to discuss findings with ED professionals and develop a framework for standardized clinical decision making.
Table 1. Multiple Variable Logisitic Regression for CSB and SW against COI
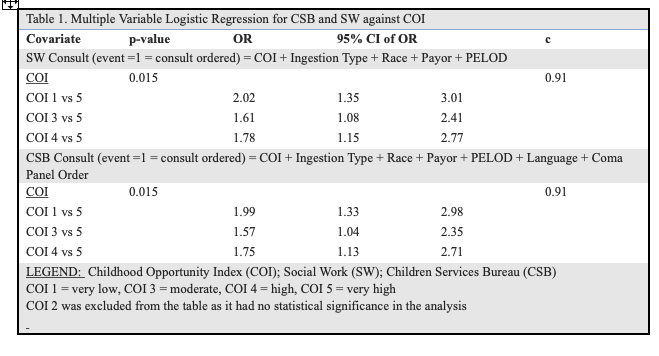 Lower COI was associated with higher odds of CSB referral and SW consult
Lower COI was associated with higher odds of CSB referral and SW consult Table 2. Multivariable Logistic Regression by Race
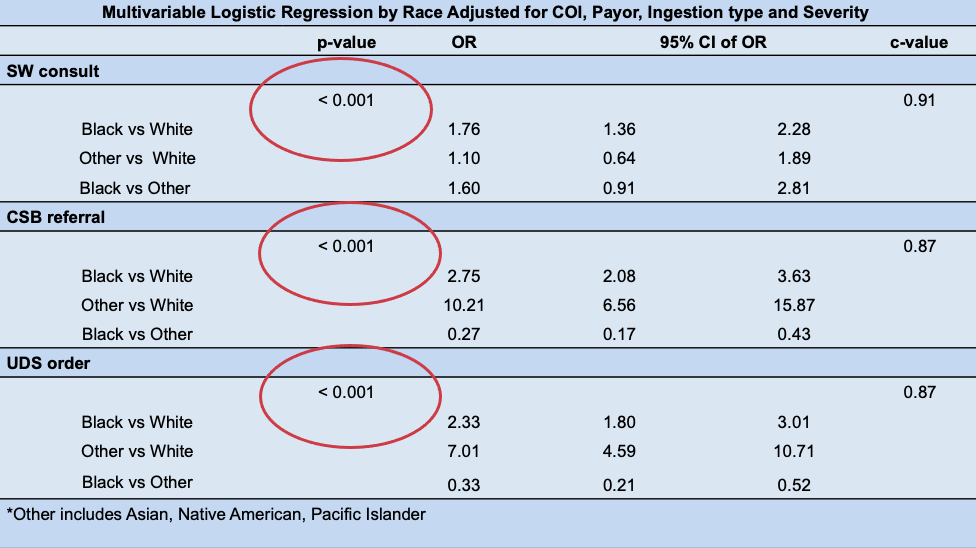 Black children had higher odds of a UDS, CSB referral and SW consult
Black children had higher odds of a UDS, CSB referral and SW consult Table 1. Multiple Variable Logisitic Regression for CSB and SW against COI
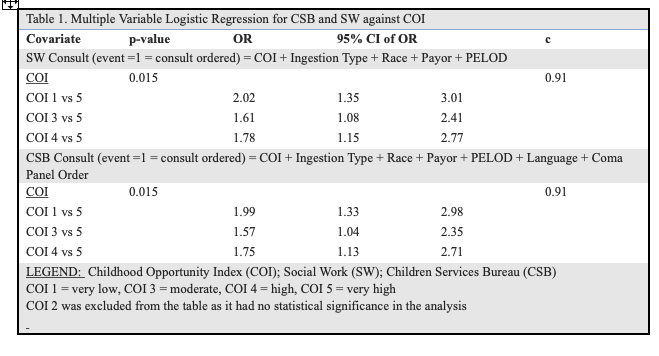 Lower COI was associated with higher odds of CSB referral and SW consult
Lower COI was associated with higher odds of CSB referral and SW consult Table 2. Multivariable Logistic Regression by Race
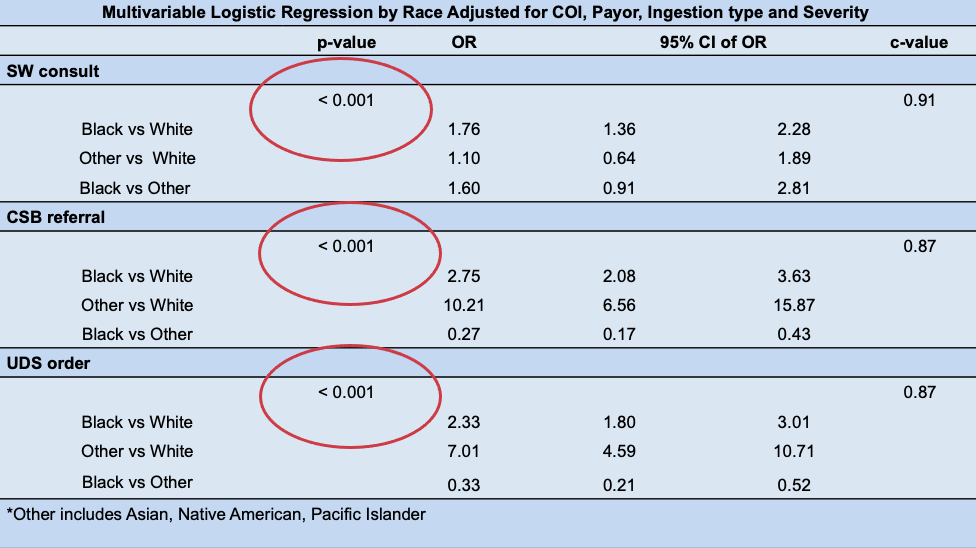 Black children had higher odds of a UDS, CSB referral and SW consult
Black children had higher odds of a UDS, CSB referral and SW consult 
