Infectious Diseases 4: Improving antibiotic use
Session: Infectious Diseases 4: Improving antibiotic use
137 - Assessing the Sustained Impact of a National QI Collaborative on Antimicrobial Stewardship Program Utilization
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 137.3836
Zoe Ziegler, University of Nebraska College of Medicine, Lansing, MI, United States; Ricky Flores, Children's Hospital & Medical Center, Bellevue, NE, United States; Alice I. Sato, UNMC; Children’s Nebraska, Omaha, NE, United States; Ellen K. Kerns, University of Nebraska Medical Center, Omaha, NE, United States; Russell J. McCulloh, University of Nebraska Medical Center, Omaha, NE, United States; Arthur Chang, University of Nebraska College of Medicine, Omaha, NE, United States

Russell J. McCulloh, MD (he/him/his)
Professor
University of Nebraska Medical Center
Omaha, Nebraska, United States
Presenting Author(s)
Background: Pediatric antimicrobial stewardship programs (pASPs) aim to decrease inappropriate antibiotic use in children. The Centers for Disease Control and Prevention (CDC) has identified core elements of ASPs, including physician accountability, pharmacy expertise, and hospital leadership commitment. Hospitalized children receive care at acute care facilities ranging from smaller community hospitals to free-standing children's hospitals; little is known about the composition of ASPs across these diverse pediatric acute care settings.
Objective: Compare hospital utilization of CDC core ASP elements before and after participation in a national QI collaborative.
Design/Methods: We conducted a pre-post comparison of ASP element use reported by hospitals participating in the American Academy of Pediatrics Better Antimicrobial Selection in Children (BASiC) quality improvement (QI) collaborative. BASiC enrolled 118 hospitals nationally 2020-2022 and aimed to improve antibiotic use for children hospitalized with community-acquired pneumonia (CAP), skin and soft tissue infection (SSTI) , or urinary tract infection (UTI). The intervention included focused education on antimicrobial stewardship and provided resources for standardizing CAP, SSTI, and UTI treatment. Sites completed an ASP program inventory based on the CDC's ASP Core Elements at baseline and project completion. Results were compared at baseline and project completion.
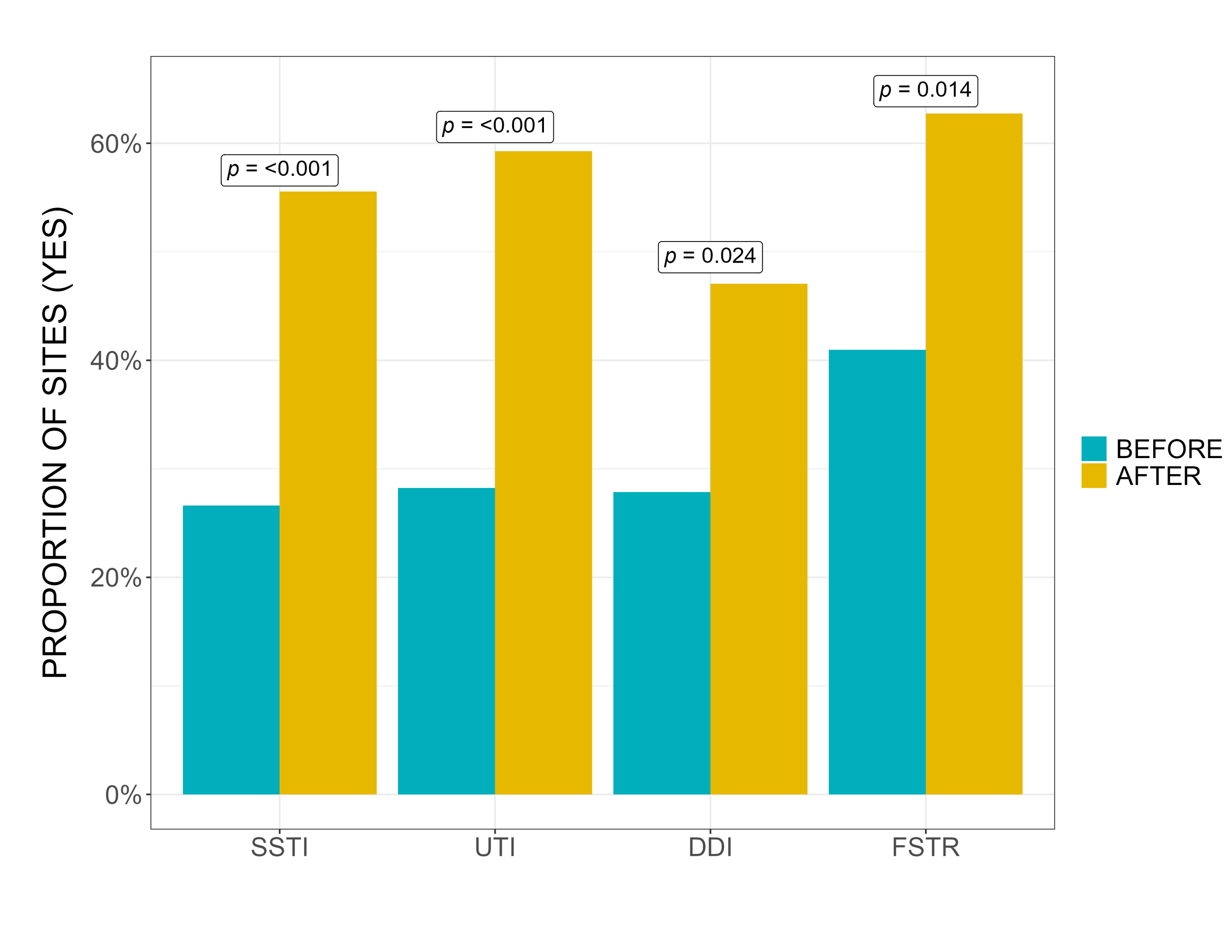
Results: 124 hospitals submitted baseline data in BASiC; 44% of sites submitted pre- and post-intervention ASP surveys (Figure 1). Fewer ASPs reported having dedicated time for program leaders to conduct daily stewardship interventions for children on antibiotics (54% ASP vs 85% pASP, p< 0.001) or providing education on optimal antibiotic prescribing to avoid adverse effects and resistance in children (47% ASP vs 80% pASP, p< 0.001). Most sites did not have treatment guidelines for pediatric CAP, SSTI, or UTI maintained by their ASP at baseline (Figure 2). ASP program elements focused on SSTI treatment, UTI treatment, documentation of duration and indication (DDI), and facility-specific treatment recommendations all increased post-intervention, which aligned with BASiC educational programming and resources provided to sites (Figure 3).
Conclusion(s): Pediatric ASPs differed from non-pediatric ASPs in components of hospital leadership and education. Increases in ASP element use aligned with BASiC interventions, suggesting that QI collaborative participation may increase institutional adoption of recommended ASP elements which may foster sustainability of improvements in antimicrobial prescribing.
Figure 1. Distribution of pASPs and ASPs from BASiC Participating Sites
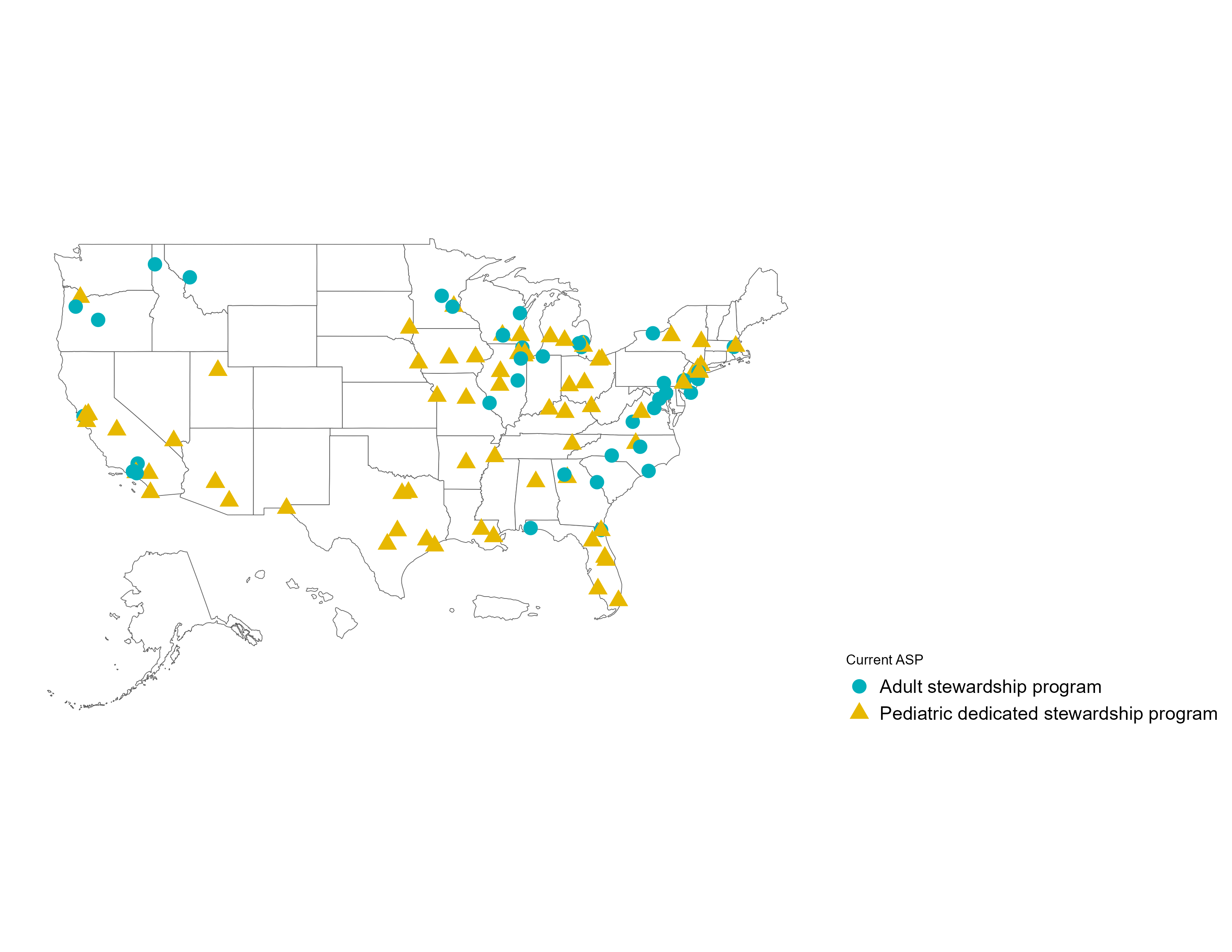 Depicted sites are limited to those that submitted both baseline and post-intervention data.
Depicted sites are limited to those that submitted both baseline and post-intervention data.Figure 2. Presence of CDC ASP Core Elements at Baseline
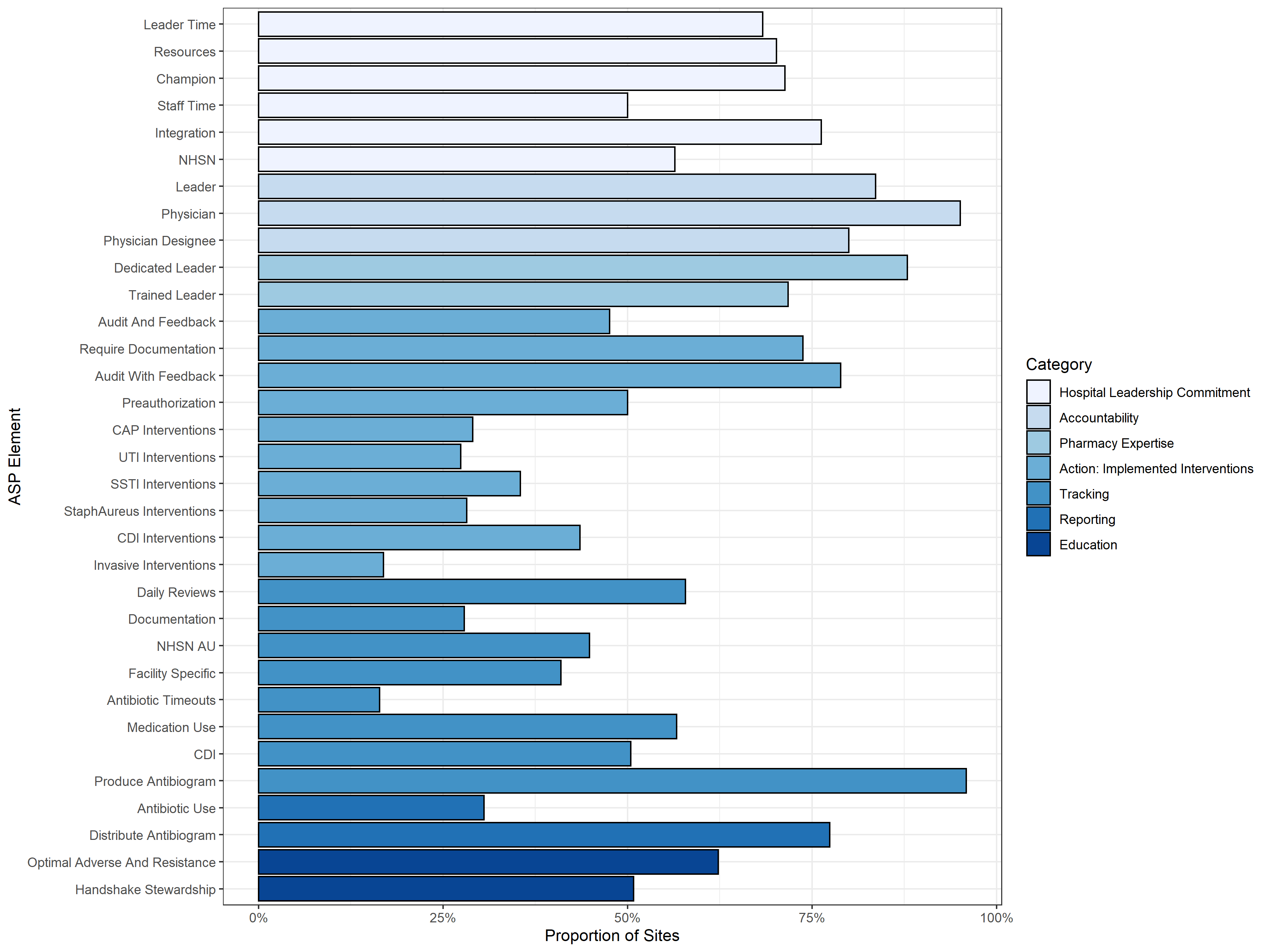
Figure 3. Changes in ASP Element Use