Emergency Medicine 4
Session: Emergency Medicine 4
244 - A Randomized Trial of ED-HEART: Emergency Department Healthcare Education Assessment and Response for Teen Relationships
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 244.3602
Kimberly A. Randell, Children's Mercy Kansas City, Kansas City, MO, United States; Melissa Miller, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Elizabeth Miller, University of Pittsburgh School of Medicine, Pittsburgh, PA, United States; Janelle Noel-MacDonnell, Children's Mercy, Kansas City, MO, United States; Ann M. Davis, University of Kansas Medical Center, KC, KS, United States; Megha Ramaswamy, University of Washington School of Public Health, Seattle, WA, United States

Kimberly A. Randell, MD, MSc (she/her/hers)
Professor of Pediatrics
Children's Mercy Kansas City
Kansas City, Missouri, United States
Presenting Author(s)
Background: Adolescent relationship abuse (ARA) is common among youth in the emergency department (ED), but current ED-based ARA interventions are limited.
Objective: Evaluate feasibility of Emergency Department Healthcare Education Assessment and Response for Teen Relationships (ED-HEART), a universal empowerment ARA intervention.
Design/Methods: We recruited youth (14-19 years) at a Midwest pediatric ED visit, randomizing participants to ED-HEART delivered privately by health educator vs enhanced usual care (standard care + resource sheet). ED-HEART uses a brief script and pocket card to empower all youth, regardless of visit reason, via education on relationship behaviors, ARA, and point of care (POC) harm reduction resources. Youth completed baseline and 12-week surveys assessing demographics, dating, ARA, ED-based ARA intervention acceptability and demand, and, in the ED-HEART arm, fidelity.
Results: We enrolled 175 participants (65% participation rate). 84.6% reported previous dating; 17.7% reported any ARA. ARA was more common among those identifying as female (83.9% vs. 16.1% males, p .001) or sexual minority (58.1% vs. 41.9% heterosexual, p < .001) or reporting sexual activity (80.6% vs. 19.4%, p < .001) (Table 1). Although most (83.9%) reporting ARA identified as cisgender, 50% identifying as gender minority reported ARA (vs. 11.6% cisgender, p .006).
Among ED-HEART participants, 13.6% requested POC resources: condoms (19), STI testing (9, emergency contraception (5), pregnancy testing (4) and social work consult (2). Two disclosed ARA to the health educator. Fidelity to the 6 core intervention components was 85.2-96.5%, (Table 2).
101 (58%; 47 ED-HEART, 54 control) completed a follow up survey. Across both arms, most rated ED-based ARA intervention as acceptable (75.6% v. 84.8%, p .156) and that they would bring a friend to the ED for ARA resources (77.8% v. 71.7%, p .480). Results suggested possible intervention benefit, although this finding is likely influenced by low follow up rates. At follow up, ED-HEART participants were less likely than control participants to report ARA (n=1 vs n=5; p .211) and more likely to report disclosing ARA to a provider at our institution (n=2 vs n=0; p .201) and that they had shared helpful resources with a friend experiencing relationship problems (93.1% vs. 78.6% , p .144) (Table 3).
Conclusion(s): Almost 1 in 5 youth in this ED sample reported ARA. Participant-reported acceptability and fidelity suggest feasibility of the ED-HEART ARA intervention. Further study with a larger sample size is warranted to evaluate efficacy of ED-HEART and its impact on youth health and ARA.
Table 1: Participant Characteristics
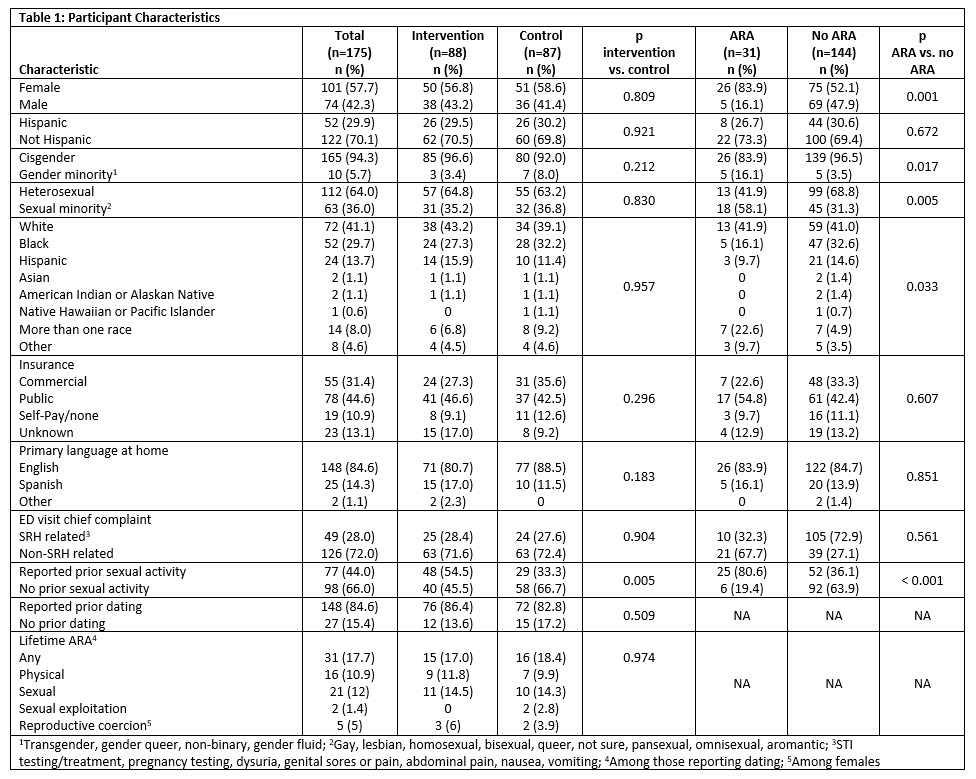
Table 2: Participant-Reported Fidelity
.png)
Table 3: Acceptability, Demand, and Efficacy
.png)
Table 1: Participant Characteristics
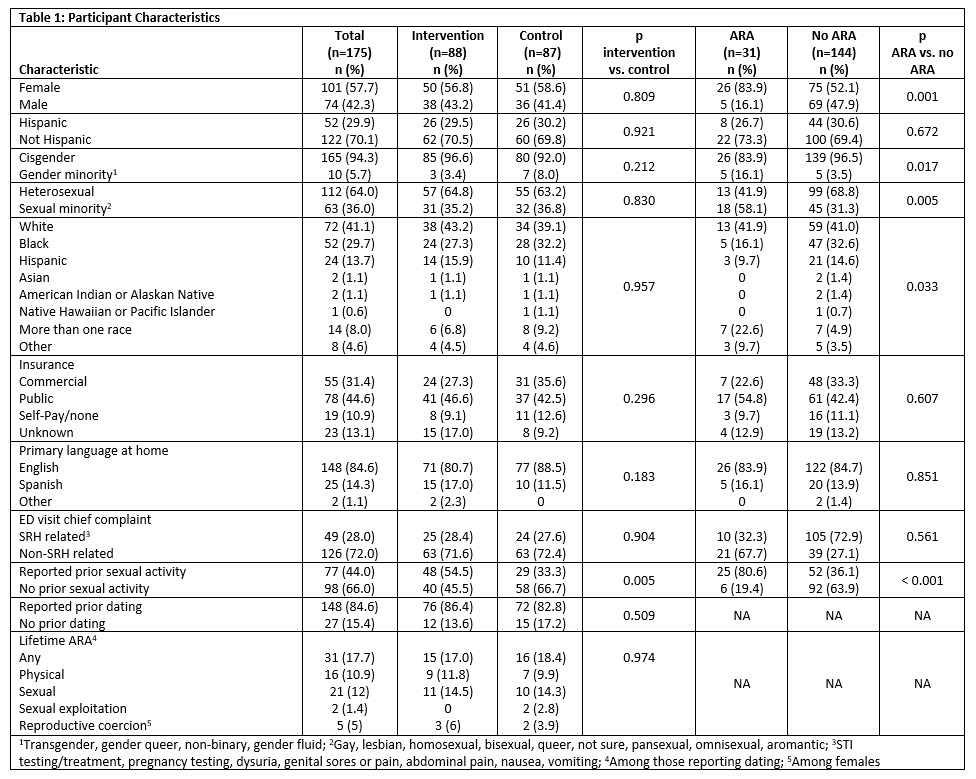
Table 2: Participant-Reported Fidelity
.png)
Table 3: Acceptability, Demand, and Efficacy
.png)

