Neonatal Nephrology/AKI 1
Session: Neonatal Nephrology/AKI 1
014 - Uncovering Patterns of Acute Kidney Injury Across Gestational Ages: A Call for Gestation-Specific Care Strategies; An ADVANCE Report
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 14.6703
Mona Khattab, Baylor College of Medicine, Houston, TX, United States; Sofia I. Perazzo, Childrens National Hospital, North Bethesda, MD, United States; Emily A. Niemyjski, Baylor College of Medicine/Texas Children’s Hospital, Houston, TX, United States; Semsa Gogcu, Women & Infants Hospital of Rhode Island, Providence, RI, United States; Andrew M. South, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Winston Salem, NC, United States; Tahagod Mohamed, Nationwide Children's Hospital, Columbus, OH, United States; Matthew W. Harer, University of Wisconsin School of Medicine and Public Health, Waunakee, WI, United States; Elizabeth Bonachea, Nationwide Children's Hospital, Columbus, OH, United States; Eileen A. Ciccia, Washington University in St. Louis School of Medicine, St. Louis, MO, United States; Thomas Nienaber, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Catherine Joseph, Baylor College of Medicine, Houston, TX, United States; Tasnim Najaf, Washington University in St. Louis School of Medicine, St. Louis, MO, United States; Michelle Starr, Indiana University School of Medicine, Indianapolis, IN, United States; Rachel Han, Riley Hospital for Children at Indiana University Health, Indianapolis, IN, United States; Cara Slagle, Indiana University School of Medicine, Indianapolis, IN, United States; Matthew C. Gillen, Emory University School of Medicine, Atlanta, GA, United States; Daniel Liu, University of Arkansas for Medical Sciences College of Medicine, Little Rock, AR, United States; Mario Schootman, University of Arkansas for Medical Sciences College of Medicine, Little Rock, AR, United States; Jonathan Bona, University of Arkansas for Medical Sciences College of Medicine, Little Rock, AR, United States; Mary E. Revenis, Children's National Health System, Chevy Chase, MD, United States; Corey Nagel, University of Arkansas for Medical Sciences, Little Rock, AR, United States; Jennifer Rumpel, Arkansas Children's Hospital, Little Rock, AR, United States
- MK
Mona Khattab, MD
Assistant Professor of Pediatrics and Neonatology
Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background: Acute Kidney Injury (AKI) is a critical complication among neonates admitted to the neonatal intensive care unit (NICU), contributing to increased mortality and potentially adverse long-term renal outcomes. The risk and clinical manifestations of AKI vary significantly across gestational ages (GA), driven by both physiologic immaturity and distinct pathological vulnerabilities at varying GA. However, data on the prevalence and severity of AKI across specific GA groups remains limited. Expanding our understanding of AKI patterns in these populations is essential to optimize care and improve neonatal outcomes. This study builds upon findings from the AWAKEN study, which examined AKI prevalence in neonates and established AKI diagnostic criteria based on serum creatinine levels and urine output.
Objective: To characterize the prevalence and severity of AKI across gestational age groups in neonates admitted to a Level IV NICU and assess the associated clinical outcomes.
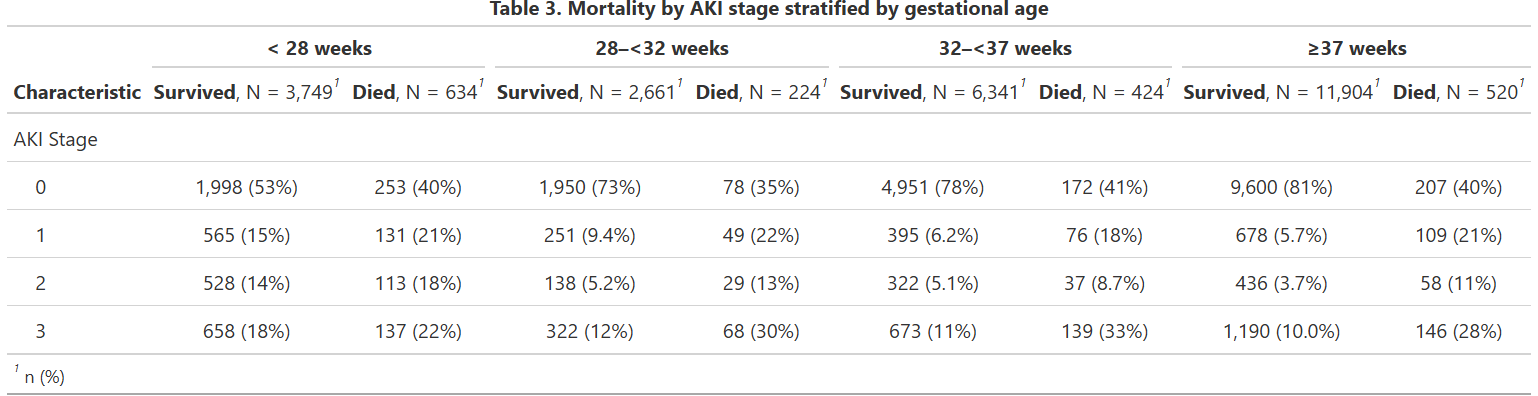
Design/Methods: This retrospective cohort study analyzed neonates admitted to the NICU between 2011 and 2023, utilizing data from the ADVANCE Database. Demographic information and in-hospital-mortality prior to one year of life were collected. Neonates were categorized by GA into the following groups: extremely preterm ( < 28 weeks), very preterm (28– < 32 weeks), moderate-to-late preterm (32– < 37 weeks), and term (≥37 weeks). AKI was identified and classified by stage according to neonatal modified KDIGO serum creatinine only criteria.
Statistical Analysis: Descriptive statistics were used to examine AKI prevalence and severity across GA categories.
Results: A total of 26,458 neonates were included in the analysis. Preliminary findings indicate that AKI prevalence was highest among extremely preterm neonates at 49% (2,133/4,384), with rates decreasing as GA increased. Stage 3 AKI prevalence was highest among extremely preterm neonates at 49% (2,133/4,384), with rates decreasing as GA increased.
Conclusion(s): AKI in the neonatal population is a substantial yet often underappreciated risk in NICU settings, with approximately half of neonates born < 28 weeks experiencing AKI. These findings support the need for NICU practices that account for gestational age-specific risks, potentially driving the development of targeted preventive strategies to improve neonatal renal care outcomes.
Table 1. Demographics By Gestational Age
.png)
Table 2. AKI status By Gestational Age
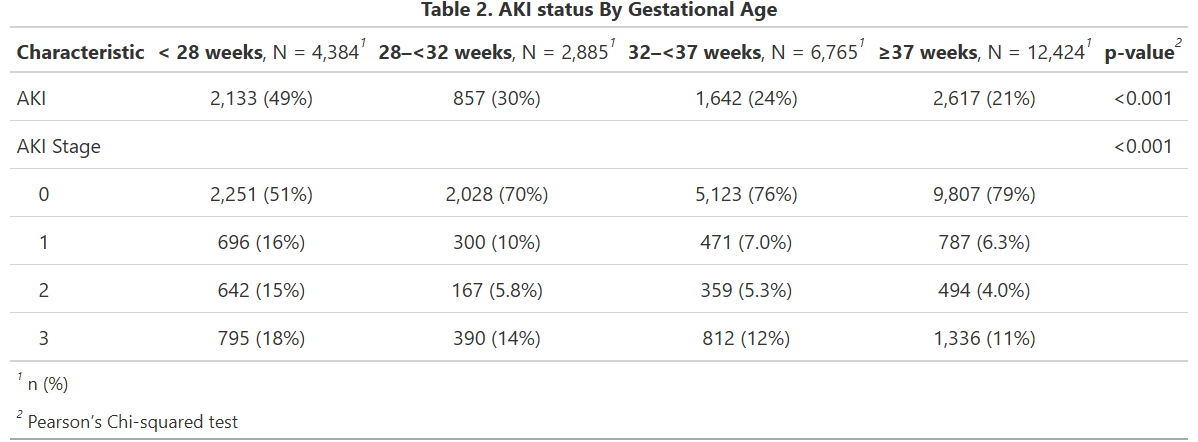
Table 3. Mortality by AKI stage stratified by gestational age