Neonatal General 7: Epidemiology, Outcomes and Periviability
Session: Neonatal General 7: Epidemiology, Outcomes and Periviability
395 - Predicting composite neonatal morbidity and mortality using metabolic profiles in preterm infants born <32 weeks gestation
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 395.6432
Kelli K. Ryckman, Indiana University, Bloomington, IN, United States; Hyunkeun Cho, University of Iowa, Iowa city, IA, United States; Nancy J. Weathers, University of Iowa Stead Family Children's Hospital, Iowa City, IA, United States; Scott P. Oltman, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; John M. Dagle, University of Iowa Stead Family Children's Hospital, Iowa City, IA, United States; Allison M. Momany, University of Iowa Stead Family Children's Hospital, Iowa City, IA, United States; Elizabeth E. Rogers, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; Laura Jelliffe-Pawlowski, New York University, New York, NY, United States
- KR
Kelli K. Ryckman, PhD
Associate Dean for Research
Indiana University
Bloomington, Indiana, United States
Presenting Author(s)
Background: The very preterm (VPT, < 32 weeks gestation) neonate is at the highest risk of developing complications that can result in significant neonatal morbidity or mortality. We have previously shown that metabolites predict major neonatal morbidity and mortality in preterm ( < 37 weeks) newborns. Further work is needed to externally validate and optimize these prediction models in VPT neonates.
Objective: To optimize and externally validate a metabolic vulnerability model for major neonatal morbidity and mortality in VPT neonates.
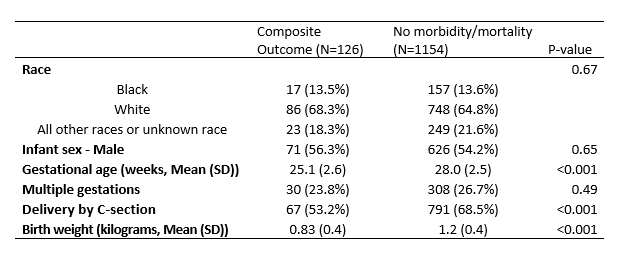
Design/Methods: Our retrospective cohort included electronic health records (EHR) for 1,280 VPT neonates born at a single Midwestern tertiary care center between 2012 and 2019. The composite outcome was defined as any major morbidity or mortality that included retinopathy of prematurity stage 3 or higher, intraventricular hemorrhage (IVH) grade 3 or higher, necrotizing enterocolitis (NEC), or death before discharge. Neonatal morbidities were identified by the International Classification of Diseases (ICD), ninth and tenth revisions. Single-variable logistic regression was performed to assess associations between forty-six metabolites measured at 24-48 hours after birth as part of routine newborn screening with the composite outcome. Metabolites were log-transformed to account for non-normal distributions. Multi-variable regression was performed to assess prediction of the composite outcome adjusting for clinical covariables including infant sex, gestational age, multiple gestation, delivery mode and birth weight.
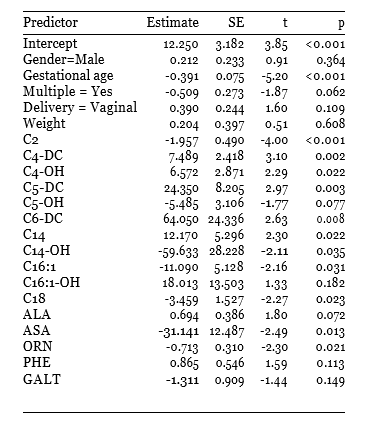
Results: There were 126 out of 1154 neonates (9.8%) that had the composite outcome. Neonates with the composite outcome were born at earlier gestational ages, were smaller at birth, and less likely to be delivered by C-section. The metabolites associated with the composite outcome included alanine (ALA), argininosuccinic acid (ASA), ornithine (ORN), phenylalanine (PHE), galactose-1-phosphate uridyl transferase (GALT) and eleven acylcarnitines (C2, C4-DC, C4-OH, C5-DC, C5-OH, C6-DC, C14, C14-OH, C16:1, C16:1-OH, and C18) (Table 2). The sensitivity of this model to predict the composite outcome was 76.3%, with a sensitivity of 81.7% and an Area Under the Curve (AUC) of 0.868.
Conclusion(s): We demonstrated that metabolic profiles could be used to predict major neonatal morbidity and mortality in VPT neonates. Using metabolic biomarkers in the prediction of neonatal morbidity and mortality has implications for improved diagnostics, clinical benchmarking, and precision treatments for the clinical management of a vulnerable population of neonates.
Demographic characteristics of the cohort.
Multivariable logistic regression analysis for composite outcome.