Neonatal GI Physiology & NEC 1
Session: Neonatal GI Physiology & NEC 1
717 - The gut microbiome in preterm infants with gastroesophageal reflux and impact of anti-reflux treatment
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 717.6843
Balpreet Singh, Dalhousie University Faculty of Medicine, Halifax, NS, Canada; Claire Carruthers, Dalhousie University Faculty of Medicine, halifax, NS, Canada; Satvinder Ghotra, IWK Health Center, Halifax, NS, Canada; Katherine A. Dunn, Dalhousie University, Halifax, NS, Canada; Sarah Organ, Dalhousie University Department of Mathematics and Statistics, Halifax, NS, Canada; Jon Dorling, University Hospital of Southampton, Southampton, England, United Kingdom

Balpreet Singh, MD, FRCPC, MSc (he/him/his)
Associate Professor
Dalhousie University
Halifax, Nova Scotia, Canada
Presenting Author(s)
Background: Adult research has shown the role of gut dysbiosis in developing Gastroesophageal reflux disease (GERD). It is crucial to determine if the same phenomenon contributes to GERD in preterm infants. Additionally, there is a need to understand how Proton Pump Inhibitors (PPI) affect preterm infants' microbiomes and contribute to infection.
Objective: 1. To compare the gut microbiome of infants with GERD versus infants with no GERD
2. Changes in the gut microbiome of infants with GERD post PPI initiation
Design/Methods: Study design, setting, population and sample size: Nested case-control study in level 3 NICU in preterm infants born less than 35 weeks gestation
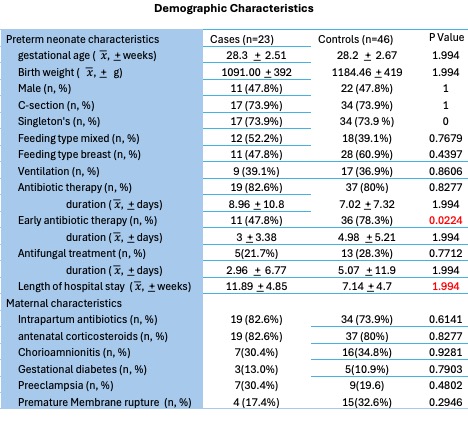
Case definition: Infants started on a PPI as cases and controls who do not have a clinical suspicion of GERD. Matching: gestational age, sex, antibiotic use, and mode of delivery. 23 cases and 46 controls
Analysis: A weekly stool sample was sequenced using 16S rRNA. Poisson principal component analysis (PPCA) was used to reduce dimensionality, and a generalized linear mixed effects model was used to account for the autocorrelation within each patient’s sample.
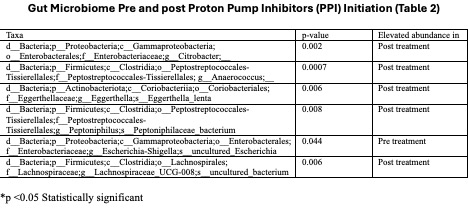
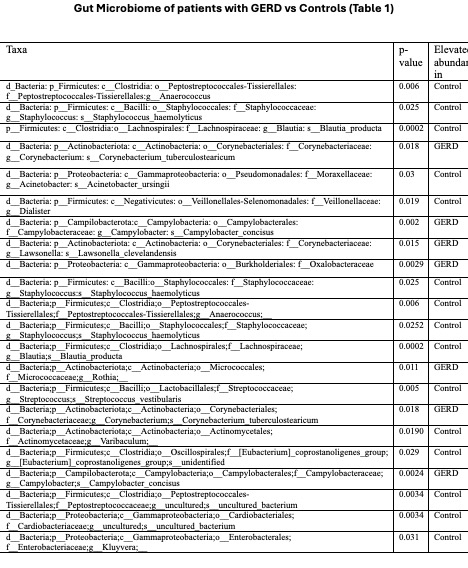
Results: The median gestational age in patients with GERD vs controls was 28.3 + 2.51 vs 28.2 ͟+ 2.67 weeks, respectively. There was a significant difference in the microbiome of patients with GERD (p < 0.006). There was an abundance of Actinobacteria (Corynebacterium tuberculostearicum, Rothia), Campylobacteria (Campylobacter concisus), and Proteobacteria (Oxalobacteriaceae) in patients with GERD, while there was an abundance of Firmicutes (Anerococcus, Staphylococcus hemolyticus, Blautia producta, Dialister, Streptococcus vestibularis, Peptostreptococcaceae), Proteobacteria (Acinetobacter ursingii, Cardiobacteriaceae, Kluyvera) and Actinobacteria (Varibaculum) in controls (Table 1). Controls had significant alpha diversity compared to patients with GERD (p= 0.033). Additionally, there was a significant change in microbiome post-PPI initiation (p < 0.001). There was an abundance of Proteobacteria (Citrobacter), Firmicutes (Enterococcus, Peptoniphilus, Lachnospiraceae UCG-008) and Actinobacteria (Eggerthella lenta) post-treatment, while there was an abundance of Proteobacteria (Escherichia) pre-treatment. (Table 2)
Conclusion(s): The results suggest significant differences in the gut microbiome in patients with GERD vs. non-GERD patients and after PPI initiation. Further studies are needed to evaluate the role of gut dysbiosis in the pathophysiology of GERD and the impact of PPI treatment-related microbiome changes on the risk of infection in this vulnerable population.
Demographic Characteristics (GERD vs Controls)
Gut Microbiome of Patients with GERD vs Controls
Gut Microbiome Pre and Post Proton Pump Inhibitors (PPI) Treatment Initiation