Neonatal Fetal Nutrition & Metabolism 2
Session: Neonatal Fetal Nutrition & Metabolism 2
629 - Growth Beyond the NICU: Nutritional and Growth Outcomes in Moderately Low Birth Weight Infants
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 629.5342
Maggie Jerome, Oregon Health and Science University, Portland, OR, United States; Arianna Kapileo, Portland State University, Portland, OR, United States; Seiji Koike, Oregon Health & Science University, Oregon City, OR, United States; Jamie B. Warren, Doernbecher Children's Hospital at Oregon Health & Science University, Portland, OR, United States
- MJ
Maggie Jerome, PhD, RD (she/her/hers)
Assistant Professor
Oregon Health & Science University School of Medicine
Portland, Oregon, United States
Presenting Author(s)
Background: Moderate and late preterm infants comprise the majority of preterm births and have twice the risk of neurodevelopmental disability at two years compared with term infants. Despite evidence linking early nutrition and growth to long-term outcomes, heterogeneity exists in feeding practices for this population and recommendations for specific nutrient intake and fortification after neonatal intensive care unit (NICU) discharge are lacking.
Objective: (1) Describe growth and feeding practices of 1500-2500 g birthweight preterm infants during the NICU stay and through 12 months of age and (2) determine the extent to which caloric intake in the NICU is predictive of growth in the first 12 months.
Design/Methods: Preterm infants with birthweights of 1500-2500 g from 2021-2023 who received NICU and primary care at Oregon Health & Science University were eligible for inclusion in this retrospective observational study. Infants with a diagnosis other than expected complications of prematurity were excluded. Dietary intake and growth data were collected from the NICU stay and at well-child visits via chart review. We measured the effect of calorie intake on day of life (DOL) 7 on changes in weight z-score to discharge using linear regression, controlling for gestational age (GA), days of respiratory support, and weight z-score on DOL 7. We also examined the effects of calorie intake at NICU discharge on the first 12-months growth trajectory using linear mixed effects models.
Results: N=75 infants weighing 2047±292 g at birth and 33 4/7 weeks ±1.56 weeks GA were included. No significant association between calorie intake on DOL 7 and change in weight z-score at discharge was found (β = 0.002; 95% CI: [-0.004, 0.009]). Due to a breakpoint in weight z-score trajectory at the first month following discharge, we modeled changes in weight using a piecewise approach, estimating separate linear slopes for pre- and post-30 days. The slope from discharge to day 30 was significant, such that an infant was predicted to increase weight z-score by 0.83 (95% CI: [0.59, 1.07]). After day 30, no significant time slope was observed (β = -0.001; 95% CI: [-0.028, 0.026]), and we found no effect of calorie intake at discharge on growth trajectories (β = -0.003; 95% CI: [-0.008, 0.002]).
Conclusion(s): Moderately low birthweight preterm infants experienced a sharp increase in weight z-score in the first month after discharge from the NICU, which was not predicted by caloric intake at discharge. More research is needed to inform nutrient recommendations post-NICU discharge to optimize development.
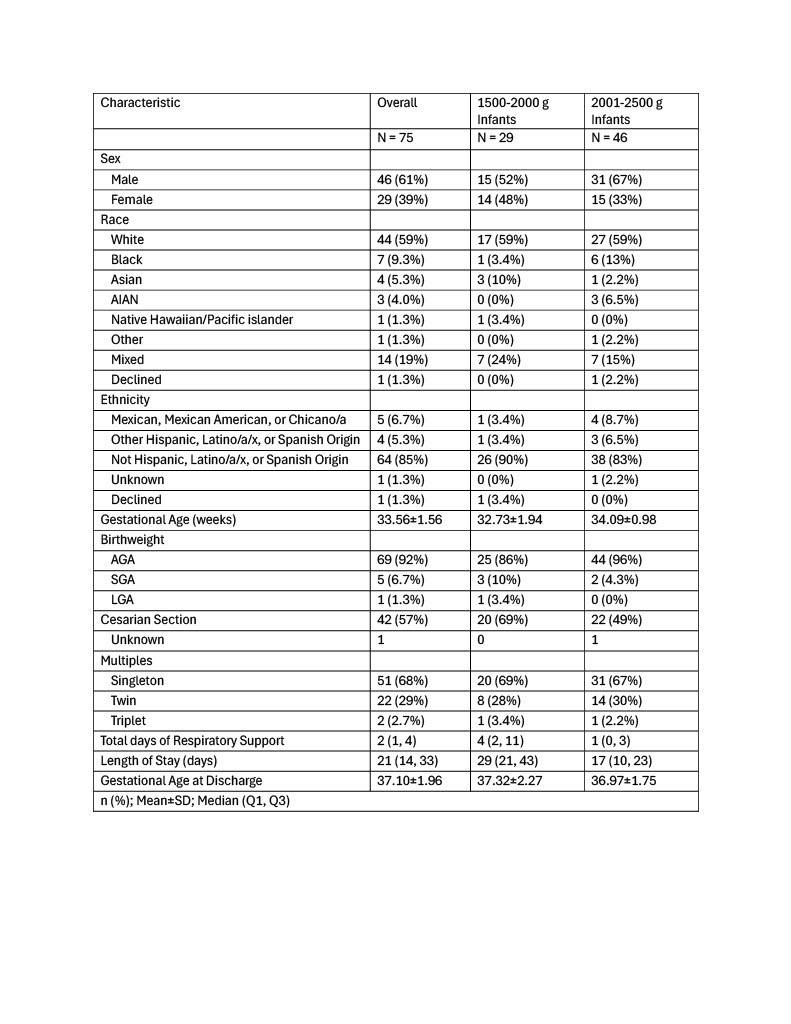
Table 1: Baseline Characteristics of Preterm Infants 1500-2500g at Birth
Tabe 2: Nutrition and Growth Outcomes
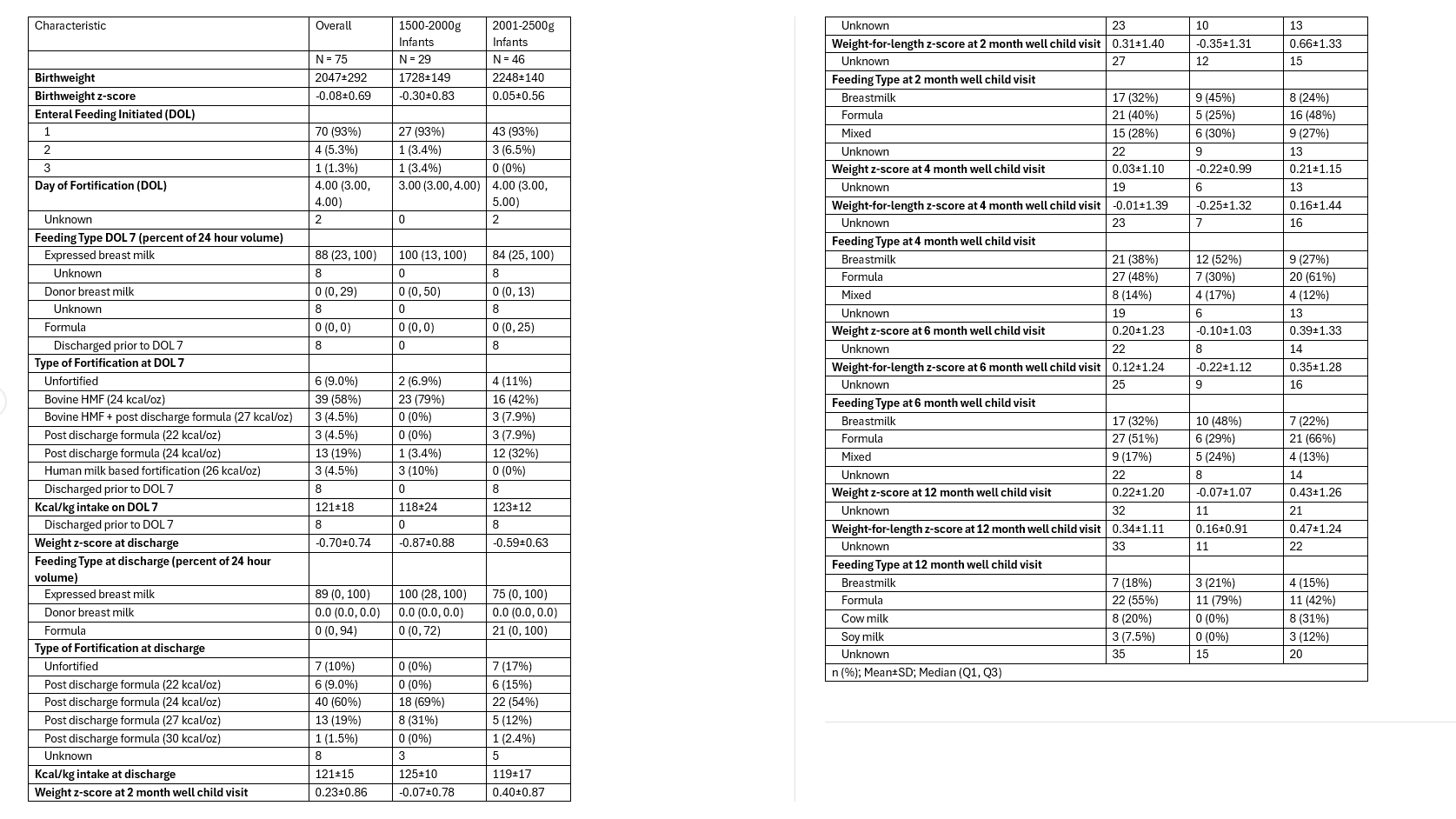
Figure 1 and 2: Weight Z-score Spaghetti Plots
.png)

