Breastfeeding/Human Milk 3
Session: Breastfeeding/Human Milk 3
665 - Intersectional Social Factors are Associated with Human Milk and Breastfeeding Outcomes for Infants with Critical Congenital Heart Disease, 2014–2023
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 665.5259
Kristin Elgersma, University of Minnesota, Minneapolis, MN, United States; Nancy Slater, Children's Hospitals and Clinics of Minnesota, Maple Grove, MN, United States; Kimberly Watkins, The Children’s Heart Clinic, Children’s Hospitals and Clinics of Minnesota, MINNEAPOLIS, MN, United States; Nellie M. Swanson, University of Minnesota, Minneapolis, MN, United States; Lynn Tanner, Children's Hospitals and Clinics of Minnesota, Minneapolis, MN, United States; Ellen W. Demerath, University of Minnesota School of Public Health, Saint Paul, MN, United States
.jpg)
Kristin Elgersma, PhD, DM (she/her/hers)
Assistant Professor
University of Minnesota
Minneapolis, Minnesota, United States
Presenting Author(s)
Background: Human milk (HM) and direct breastfeeding (BF) benefit infants with critical congenital heart disease (CCHD). While social factors impact HM/BF rates for infants with CCHD, the intersectional effect of these factors is unknown.
Objective: We aimed to describe single-site trends in HM/BF for infants with CCHD over 10 years, and to compare discharge HM outcomes among intersectional social strata (ie, subgroups).
Design/Methods: We included infants ≥32 weeks undergoing neonatal CCHD surgery from 2014–2023. We applied an intersectional multilevel analysis of individual heterogeneity and discriminatory accuracy (I-MAIHDA) framework to compare HM outcomes among social strata, including infant race, insurance type, and a composite socioeconomic (SES) score based on the Child Opportunity Index, the Mayo Clinic HOUSES index, and the Area Deprivation Index.
Results: Infants (n=363) were 36.9% female, 67.0% White, and 41.3% with public insurance. Diagnoses included 35.5% single ventricle physiology. Most (89.7%) parents planned to provide HM (77.6% exclusive) and BF (80.1%).
At discharge, rates of any HM/any BF were 76.8%/36.8% in the full sample and 84.1%/44.3% (49.1% exclusive HM) for those with a documented HM/BF goal. There were no observable trends in discharge HM/BF rates from 2014–2023 (range, 60.0%–88.9% HM; 26.7%–42.4% BF; see Figure 1).
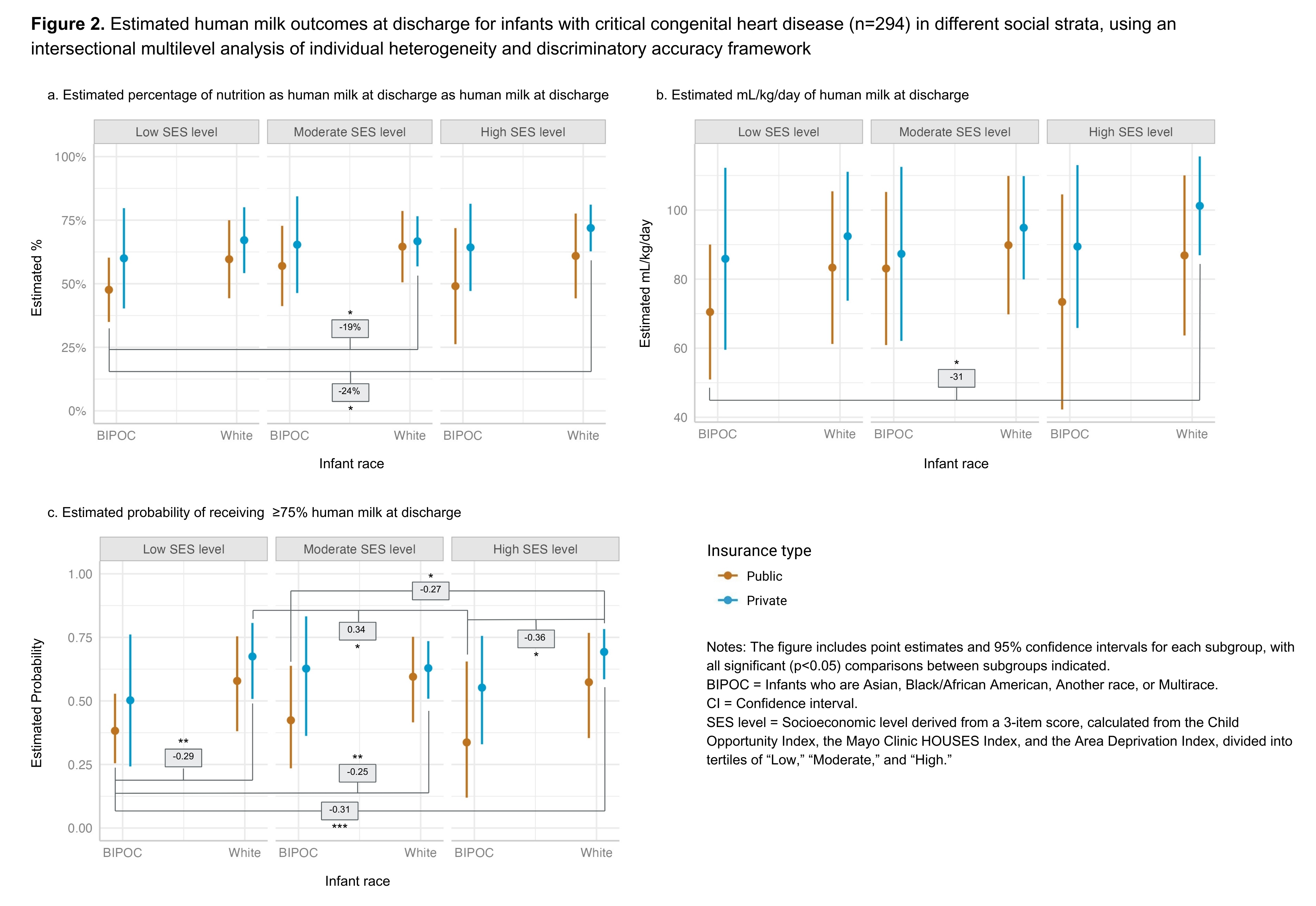
In regression models adjusted for hospital length of stay, social factors were individually associated with HM/BF outcomes (Table 1). Significant differences in HM estimates at discharge, by intersectional social strata, can be seen in Figure 2. Infants in the Black, Indigenous, People of Color (BIPOC)/public insurance/low SES stratum had lower HM at discharge compared to multiple other strata. For example, these infants received 24% less nutrition as HM (p=0.002) – an average 31 mL/kg/day less (p=0.013) – and were 31% less likely to receive ≥75% HM at discharge (p < 0.001), compared to infants in the White/private insurance/high SES stratum. These infants were also less likely to receive ≥75% HM at discharge than infants in White/private insurance strata at both the low SES (29% lower, p=0.006) and moderate SES (25% lower, p=0.008) levels.
Conclusion(s): While most parents planned to BF and provide exclusive HM, many did not reach these goals by discharge. Intersectional social factors were associated with HM at discharge. Infants with CCHD who are BIPOC, with public insurance, and with a low SES score may be at risk for poor HM outcomes. Interventions to assist parents in reaching their HM/BF goals are needed, including strategies to effectively support high-risk families.
Figure 1. Ten-year trends in human milk and breastfeeding outcomes at discharge
.jpg)
Table 1. Regression models to estimate associations between SES level, race, or insurance type on lactation outcomes at discharge, adjusted for neonatal length of stay
.jpg)
Figure 2. Estimated human milk outcomes at discharge for infants with critical congenital heart disease (n=294) in different social strata, using an intersectional multilevel analysis of individual heterogeneity and discriminatory accuracy framework