Neonatal Fetal Nutrition & Metabolism 2
Session: Neonatal Fetal Nutrition & Metabolism 2
618 - Impact of parental and perinatal risk factors on type 1 DM based on different endotypes
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 618.5347
Yin-Ting Chen, China Medical University Children's Hospital, Taiwan, Taichung, Taichung, Taiwan (Republic of China); Yu-Chia chang, National Quemoy University, Kinmen County, Kinmen, Taiwan (Republic of China); Hsin-Ru Wu, China medical university children's hospital, Taichung, Taichung, Taiwan (Republic of China); Hung-Chih Lin, China Medical University Children's Hospital, Taichung City, Taichung, Taiwan (Republic of China); Shang-Po Shen, ChinaMedical University Children’s Hospital, Taichung city, Taichung, Taiwan (Republic of China)
.jpg)
Yin-Ting Chen, MD (she/her/hers)
Attending Physician
China Medical University Children's Hospital, Taiwan
Taichung, Taichung, Taiwan (Republic of China)
Presenting Author(s)
Background: Type 1 diabetes mellitus (T1DM) is an autoimmune disease with both genetic and environmental factors, often emerging in early childhood or pre-adolescence. Recent studies link perinatal factors like preterm birth and parental autoimmune diseases to elevated T1DM risk. The risk may vary with age at onset, indicating potential early-onset (genetically influenced) and late-onset (environmentally influenced) T1DM types. This study uses Taiwan’s health insurance data to analyze perinatal risk factors across T1DM onset ages.
Objective: This study evaluates perinatal risk factors for T1DM in children, distinguishing early-onset from non-early onset cases. We hypothesize that early-onset T1DM is more genetically influenced, while non-early onset T1DM may have stronger environmental associations.
Design/Methods: Taiwan’s National Health Insurance Research Database provided data on individuals born 2004-2022 with T1DM diagnoses (excluding first-year diagnoses). Each case was matched 1:5 with healthy controls by birth year and weight. We assessed perinatal risk factors using logistic regression to compare early-onset ( < 8 years) and non-early onset T1DM with controls.
Results: The analysis included 1,766 T1DM cases, with 909 classified as early-onset and 858 as non-early onset. Compared to healthy controls, risk factors for total T1DM included female sex (OR 1.36), late preterm birth (OR 1.32), maternal T1DM (OR 7.62), maternal type 2 diabetes (OR 1.84), and maternal autoimmune diseases (OR 2.30). Cesarean delivery was linked to a reduced risk (OR 0.88). For early-onset T1DM, risk factors included female sex (OR 1.27), maternal T1DM (OR 19.41), paternal type 2 diabetes (OR 1.82), and maternal autoimmune diseases (OR 2.26), with maternal hypertension showing a protective effect (OR 0.57). In contrast, for non-early onset T1DM, risk factors included female sex (OR 1.48), late preterm birth (OR 1.45), and maternal type 2 diabetes (OR 3.30), with cesarean delivery again serving as a protective factor (OR 0.82).
Conclusion(s): This study shows that perinatal risk factors associated with T1DM vary by age of onset, supporting the existence of age-specific T1DM subtypes. Maternal and paternal diabetes links, particularly maternal T1DM, underscore the genetic influences in early-onset cases, while environmental factors may play a greater role in non-early onset T1DM. The findings highlight the need for age-specific risk stratification and suggest further exploration into genetic-environmental interactions could improve T1DM prediction and prevention strategies.
Image 1. Incidence of type 1 diabetes by age in Taiwan (2004–2020)
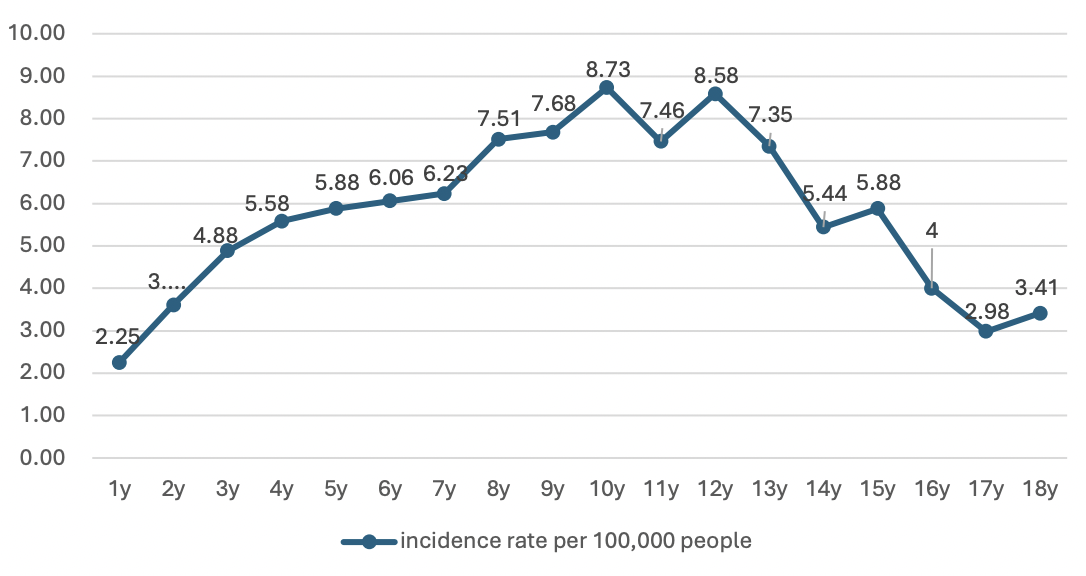 Highlighting prominent onset peaks in early childhood and pre-adolescence.
Highlighting prominent onset peaks in early childhood and pre-adolescence.Table 2. Risk factors of incident early T1DM ( < 8 years old)
.png) For early-onset T1DM, risk factors included female sex (OR 1.27, 95% CI: 1.08-1.44), maternal T1DM (OR 19.41, 95% CI: 3.52-107.22), paternal type 2 diabetes (OR 1.82, 95% CI: 1.09-3.05), and maternal autoimmune diseases (OR 2.26, 95% CI: 1.06-4.81), with maternal hypertension as a protective factor (OR 0.57, 95% CI: 0.36-0.91).
For early-onset T1DM, risk factors included female sex (OR 1.27, 95% CI: 1.08-1.44), maternal T1DM (OR 19.41, 95% CI: 3.52-107.22), paternal type 2 diabetes (OR 1.82, 95% CI: 1.09-3.05), and maternal autoimmune diseases (OR 2.26, 95% CI: 1.06-4.81), with maternal hypertension as a protective factor (OR 0.57, 95% CI: 0.36-0.91).Table 3. Risk factors of incident non-early T1DM (8+ years old).
.png) For non-early onset T1DM, female sex (OR 1.48, 95% CI: 1.28-1.74), late preterm birth (OR 1.45, 95% CI: 1.11-1.88), and maternal type 2 diabetes (OR 3.30, 95% CI: 1.66-6.57) were risk factors, with cesarean delivery as a protective factor (OR 0.82, 95% CI: 0.70-0.97).
For non-early onset T1DM, female sex (OR 1.48, 95% CI: 1.28-1.74), late preterm birth (OR 1.45, 95% CI: 1.11-1.88), and maternal type 2 diabetes (OR 3.30, 95% CI: 1.66-6.57) were risk factors, with cesarean delivery as a protective factor (OR 0.82, 95% CI: 0.70-0.97). 
