Neonatal Fetal Nutrition & Metabolism 2
Session: Neonatal Fetal Nutrition & Metabolism 2
625 - Nutrition in Infants with Hypoxic-Ischemic Encephalopathy: Insights from a Single-Center Experience on Parenteral and Enteral Feeding During Therapeutic Hypothermia
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 625.5903
Isaura Molina Stornelli, University of Florida College of Medicine, Metairie, LA, United States; Nikolay Bliznyuk, University of Florida, Gainesville, FL, United States; Juan C.. Roig, University of Florida, Gainesville, Gainesville, FL, United States; Michael D. Weiss, University of Florida College of Medicine, Gainesville, FL, United States; Josef Neu, University of Florida College of Medicine, Gaineville, FL, United States; Katherine E. Kisilewicz, UF Health Shands Children's Hospital, Gainesville, FL, United States

Isaura Molina Stornelli, MD (she/her/hers)
Neonatologist
Ochsner Medical Center
Flushing Hospital Medical Center
Metairie, Louisiana, United States
Presenting Author(s)
Background: Therapeutic hypothermia (TH) is the standard of care for neonates with hypoxic-ischemic encephalopathy (HIE). While fluid restriction with intravenous dextrose is commonly employed during TH, limited evidence regarding optimal nutritional strategies during TH remains unclear. This study compared intravenous fluids (IVFs), parenteral nutrition (PN), and a combination (MIX) to determine the best approach for metabolic stability and neurodevelopmental support. We hypothesized PN would improve metabolic health and neurodevelopmental outcomes than IVF alone. Further, we proposed that neonates receiving enteral feeds would show better recovery and developmental outcomes.
Objective: This study aims to inform clinical practice by identifying effective nutritional strategies to enhance recovery and optimize outcomes for neonates undergoing TH.
Design/Methods: This single-center retrospective study included 163 neonates treated with TH for HIE between 2012 and 2020, categorized by primary nutrition strategy: IVFs, PN, or MIX. Further analyses compared neonates who received enteral feeds to those who did not, evaluating the impact on brain MRI injury, growth metrics, and neurodevelopmental outcomes as assessed by Bayley-III scores. Group differences were assessed using ANOVA and Kruskal-Wallis tests.
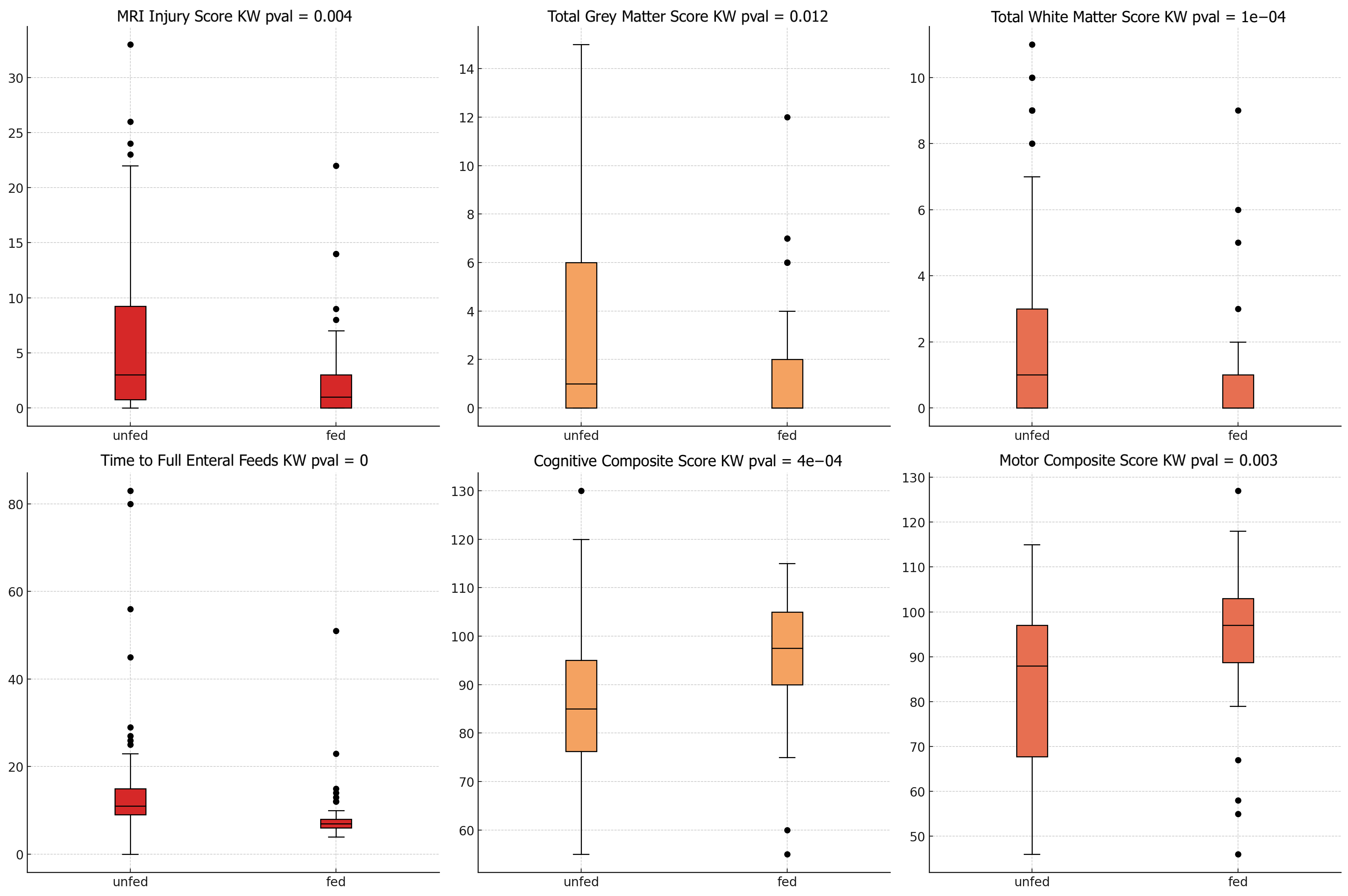
Results: PN was associated with improved glucose regulation at 12 hours (p=0.02) and higher BUN levels across all time points examined during TH (p < 0.05), though clinically acceptable. MRI analysis revealed that neonates receiving enteral feeds had significantly lower total MRI injury scores (p=0.004), with specific reductions in grey matter (p=0.012) and white matter injury scores (p=0.0001). Additionally, the fed group showed higher cognitive (p=0.0004) and motor Bayley scores (p=0.003), reached full feeds faster (p < 0.05), had shorter NICU stays (p=0.02), and experienced fewer seizures (p=0.04). Maternal breast milk was the primary enteral feed, accounting for 47% of initial feedings.
Conclusion(s): Early nutrition, including PN and enteral feeding, appears feasible, well-tolerated, and may support recovery and neurodevelopment in neonates undergoing TH. Integrating PN with enteral feeds shows potential for promoting metabolic stability and may contribute to neuroprotective benefits, as suggested by lower MRI injury scores in enterally-fed infants. These findings provide insights that could guide clinical practice and help optimize nutritional strategies during TH.
Figure 1: BUN Levels Over Time during TH by Nutrition Type (IVF, MIX, TPN)
.png)
Figure 2: MRI Injury Scores and Bayley Developmental Scores in Neonates Fed vs. Unfed During TH.
Baseline Demographics and Clinical Characteristics of Neonates with HIE Undergoing TH
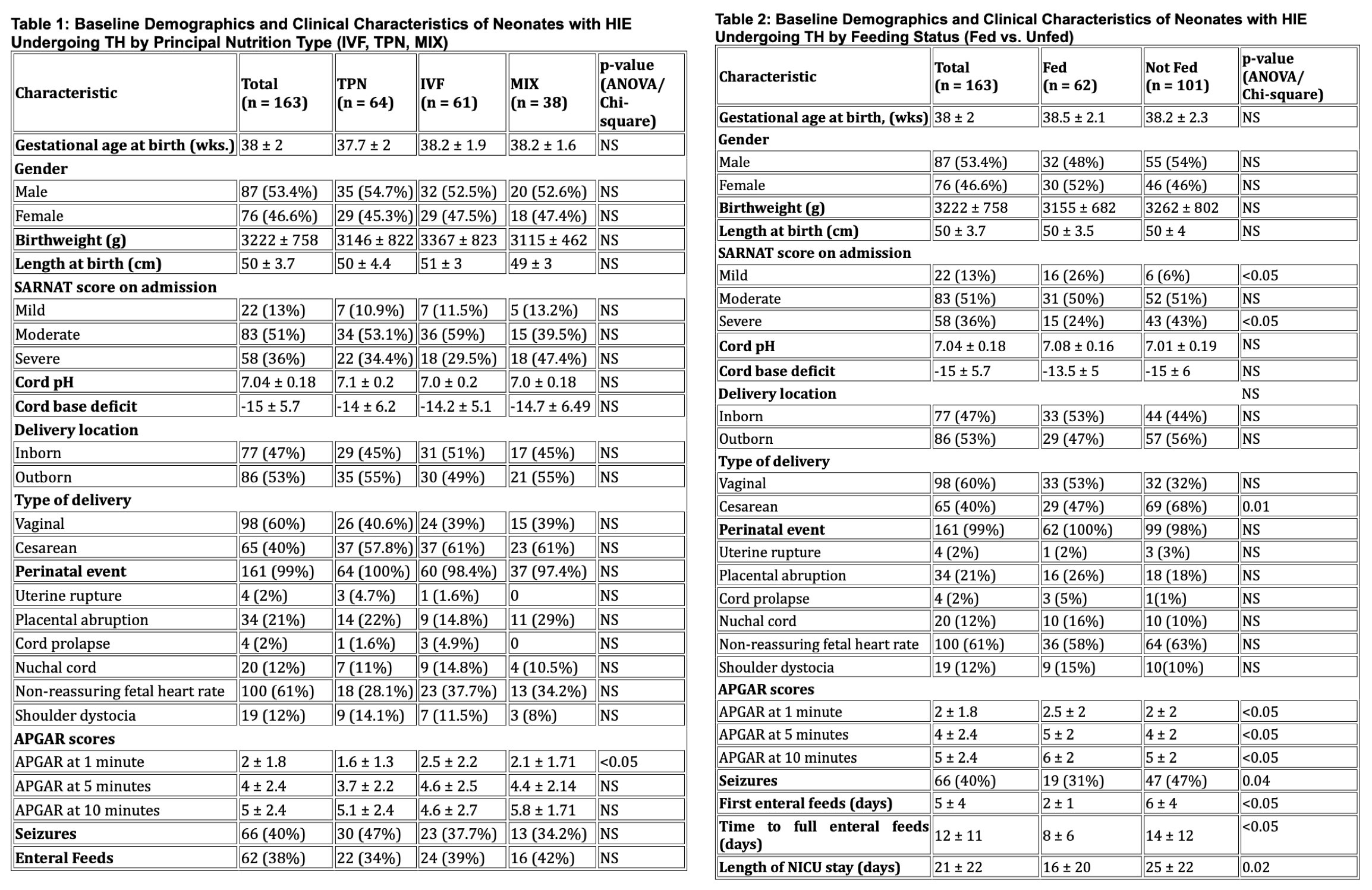 Table 1: By Principal Nutrition Type (IVF, TPN, MIX)
Table 1: By Principal Nutrition Type (IVF, TPN, MIX)Table 2: By Feeding Status (Fed vs. Unfed)

