Global Neonatal & Children's Health 4
Session: Global Neonatal & Children's Health 4
771 - Barriers and facilitators to telehealth for newborn resuscitation in the Democratic Republic of the Congo
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 771.3582
Amy Mackay, University of Alabama at Birmingham School of Medicine, Birmingham, AL, United States; Daniel Ishoso, Kinshasa School of Public Health, Kinshasa, Kinshasa, Congo, (Congo – Kinshasa); Ingunn A. Haug, Laerdal Medical, Sandnes, Rogaland, Norway; Tonje S. Birkenes, Laerdal Medical, Stavanger, Rogaland, Norway; Eric Musalu. Mafuta, Ecole de Santé Publique de Kinshasa/UNIKIN, Kinshasa, Kinshasa, Congo, (Congo – Kinshasa); Jackie Patterson, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC, United States

Amy Mackay, MD, MPH (she/her/hers)
Assistant Professor
University of Alabama at Birmingham School of Medicine
Birmingham, Alabama, United States
Presenting Author(s)
Background: Evidence-based neonatal resuscitation is challenging, especially for providers with limited opportunity to practice bag-mask ventilation in clinical care. Coaching by a physician during resuscitation may improve care, but the limited availability of resuscitation experts may preclude implementation in low-resource settings. Telehealth is one strategy that can be used to extend coaching to these settings.
Objective: Explore the barriers and facilitators of coaching via telehealth for neonatal resuscitation among Congolese midwives and physicians
Design/Methods: To engage with midwives and physicians regarding barriers and facilitators to telehealth, we conducted four simulated newborn resuscitations during which a physician provided coaching to a midwife using Zoom. We analyzed the video footage of the simulations based on an analysis plan developed a priori. Following simulations, the local study physician conducted one 90-minute focus group discussion (FGD) with five midwives and semi-structured interviews with two physicians in French. The FGD and interviews were audio-recorded and transcribed. Using qualitative content analysis, AM coded the French transcripts using NVivo (Lumivero, release 14.23.3). Two coders (AM and JP) independently created English clusters of codes to identify patterns in the data, grouped clusters into themes, and determined final themes by consensus.
Results: Simulation video analysis revealed that midwives largely followed physician instructions, and communication was predominantly from the physician to the midwife. We identified several themes from the FGD and interviews: Midwives reported issues related to integrating the technology around laboring mothers as a potential barrier, while physicians reported human resources for coaching as a potential barrier. Both reported establishing a trusting relationship between the coach and midwives as a facilitator, and physicians reported financial incentives to coaches as a facilitator. Midwives reported reinforcement of training as a potential benefit, while physicians reported capacity building as a potential benefit. Both reported a potential pitfall, or harm could occur if providers (coach or midwife) did not have sufficient training
Conclusion(s): Midwives and physicians expressed a shared belief in the potential of telehealth for newborn resuscitation to enhance care. Implementing telehealth in this setting may require building relationships between midwives and physicians, financial incentives to motivate physicians in understaffed environments, and resources to ensure consistent internet/power.
Figure: Resuscitation simulations with remote coaching
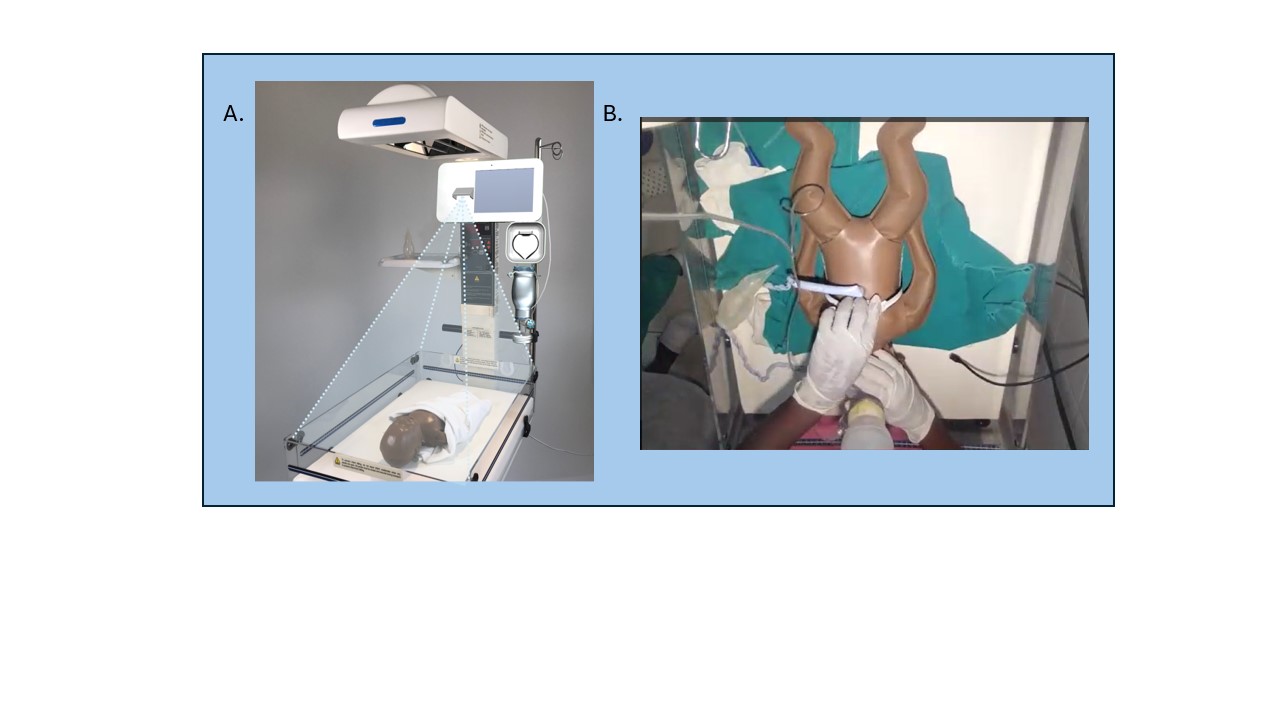 We conducted simulated resuscitations using the Liveborn Station and Neonatalie Live (A). Liveborn Station is a warmer bed with an embedded tablet for video recording, a penguin suction, an upright bag and mask, and NeoBeat (a battery-operated heart rate meter). NeoNatalie Live is a high-fidelity manikin with four programmed scenarios of varying lung compliance. During simulations, the coach connected with the midwife via Zoom (B) to visualize the resuscitation and provide advice.
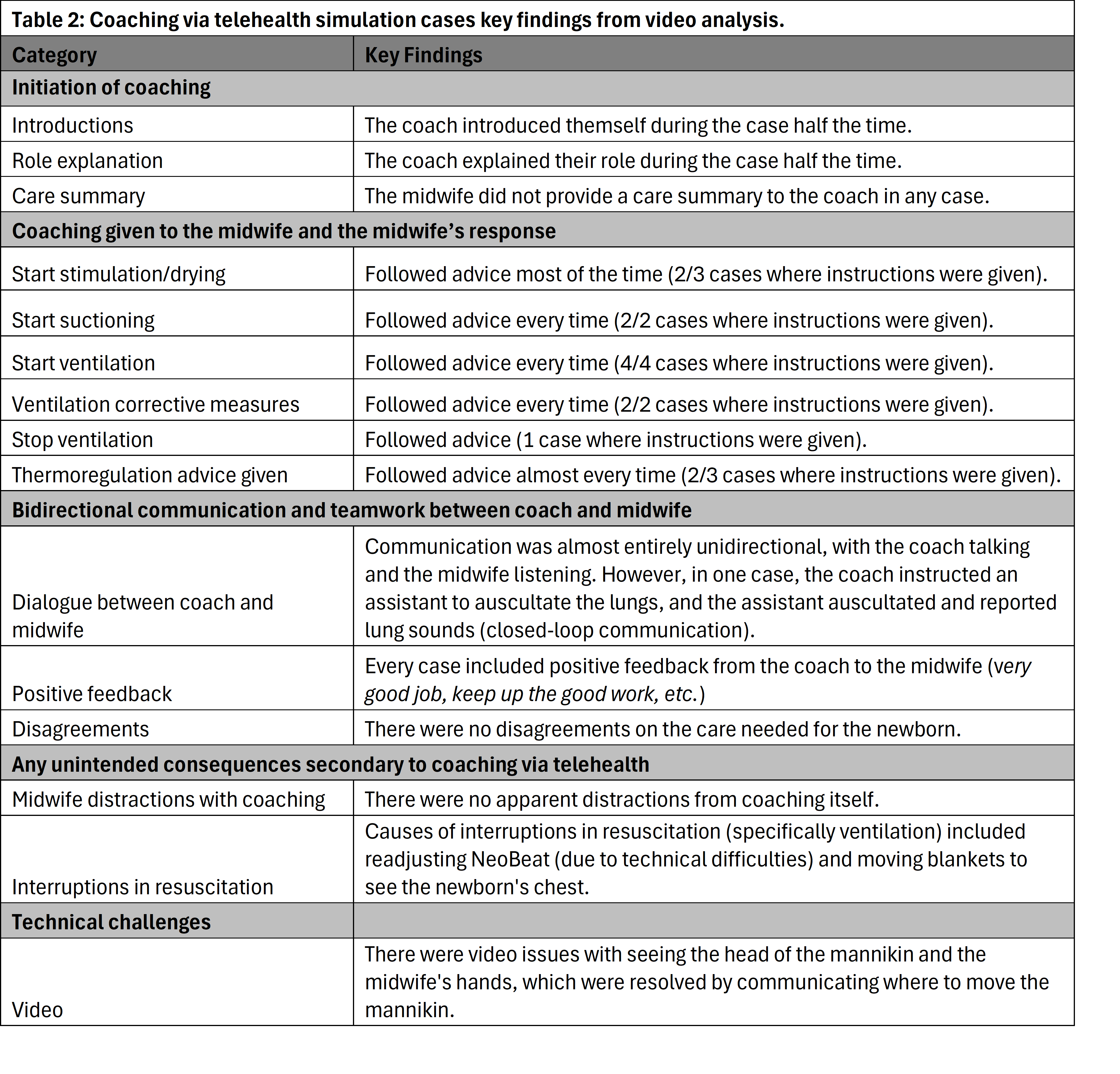
We conducted simulated resuscitations using the Liveborn Station and Neonatalie Live (A). Liveborn Station is a warmer bed with an embedded tablet for video recording, a penguin suction, an upright bag and mask, and NeoBeat (a battery-operated heart rate meter). NeoNatalie Live is a high-fidelity manikin with four programmed scenarios of varying lung compliance. During simulations, the coach connected with the midwife via Zoom (B) to visualize the resuscitation and provide advice. Table 1: Illustration of qualitative content analysis with themes, exemplary clusters and quotes
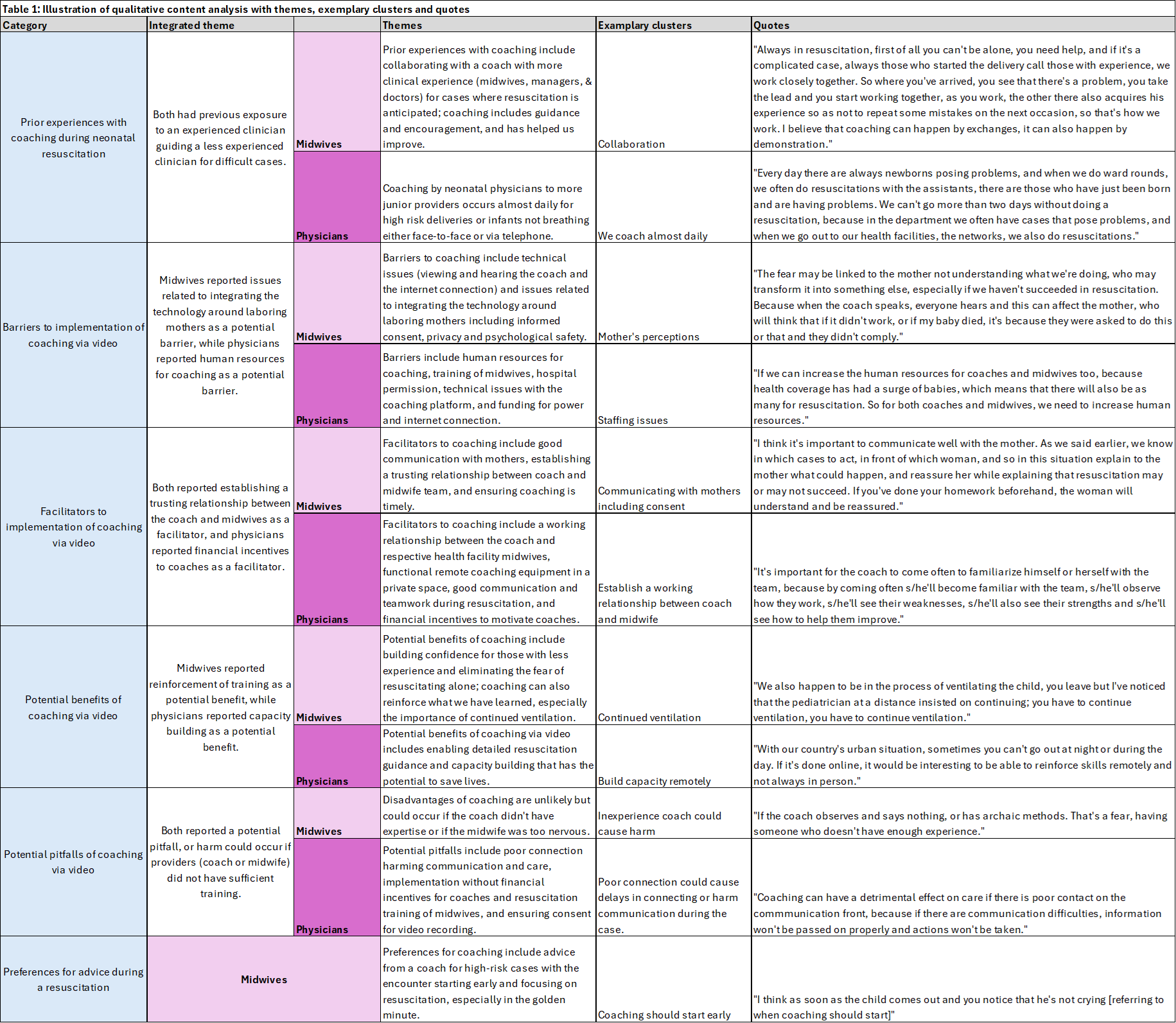
Table 2: Coaching via telehealth simulation cases key findings from video analysis.
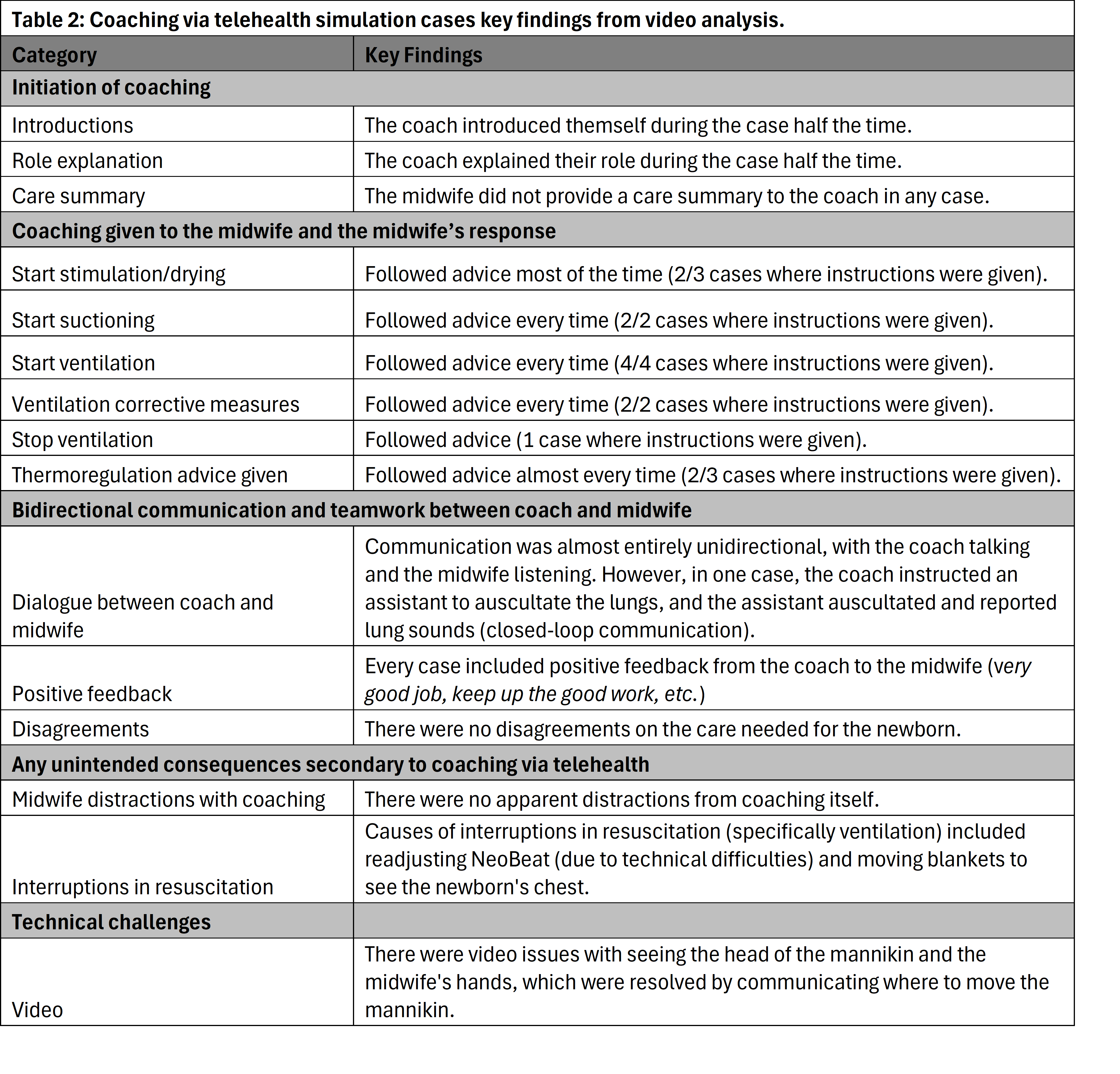
Figure: Resuscitation simulations with remote coaching
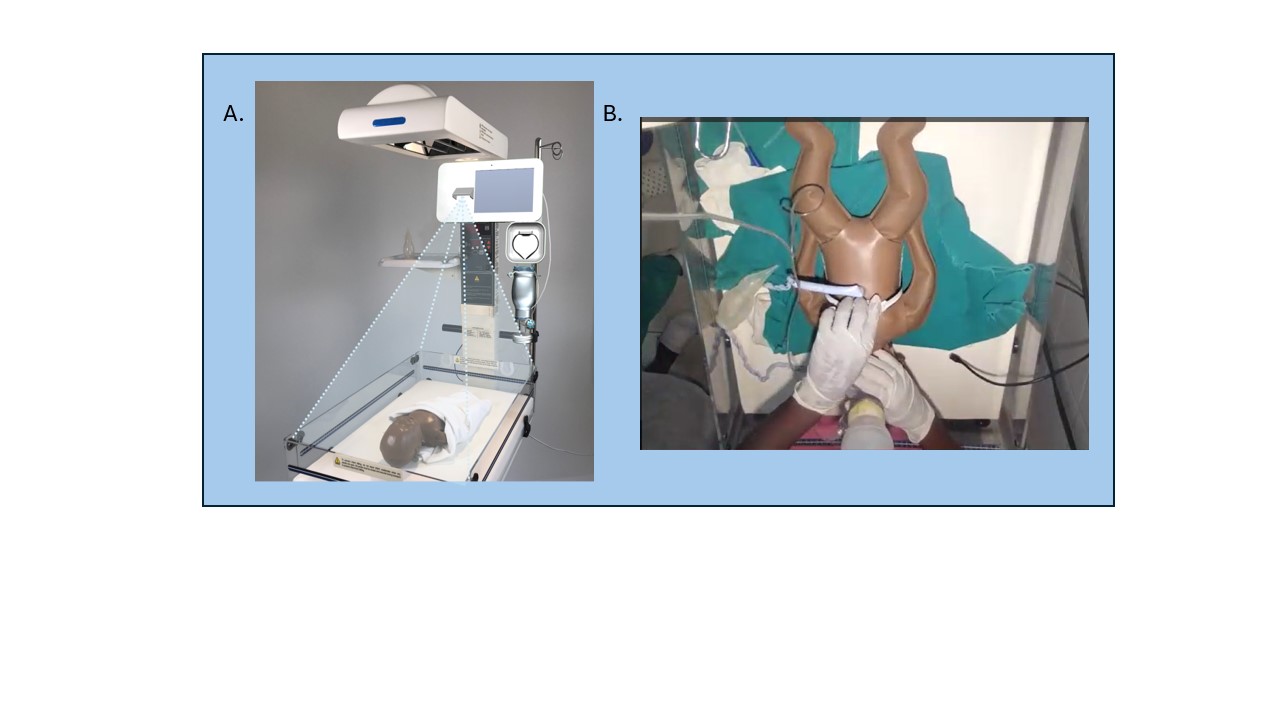 We conducted simulated resuscitations using the Liveborn Station and Neonatalie Live (A). Liveborn Station is a warmer bed with an embedded tablet for video recording, a penguin suction, an upright bag and mask, and NeoBeat (a battery-operated heart rate meter). NeoNatalie Live is a high-fidelity manikin with four programmed scenarios of varying lung compliance. During simulations, the coach connected with the midwife via Zoom (B) to visualize the resuscitation and provide advice.
We conducted simulated resuscitations using the Liveborn Station and Neonatalie Live (A). Liveborn Station is a warmer bed with an embedded tablet for video recording, a penguin suction, an upright bag and mask, and NeoBeat (a battery-operated heart rate meter). NeoNatalie Live is a high-fidelity manikin with four programmed scenarios of varying lung compliance. During simulations, the coach connected with the midwife via Zoom (B) to visualize the resuscitation and provide advice. Table 1: Illustration of qualitative content analysis with themes, exemplary clusters and quotes
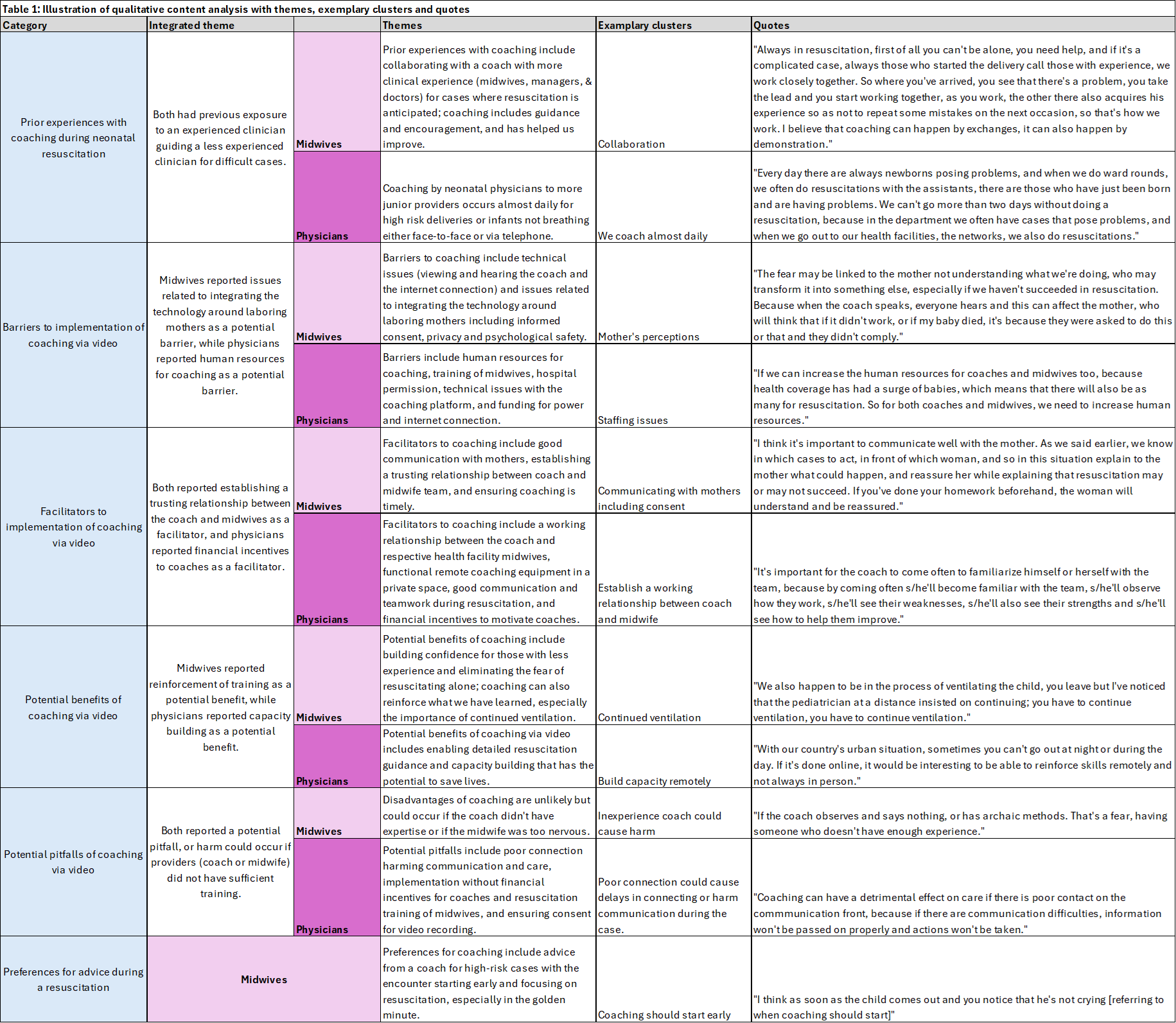
Table 2: Coaching via telehealth simulation cases key findings from video analysis.