Obesity 2
Session: Obesity 2
282 - Behavioural components and delivery features of early childhood obesity prevention interventions: a systematic review and intervention coding of studies in the TOPCHILD Collaboration
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 282.3701
Brittany J. Johnson, Flinders University, Bedford Park, South Australia, Australia; Paul Chadwick, university college london, Washington, DC, United States; Samantha pryde, Flinders University, Adelaide, South Australia, Australia; Anna Lene Seidler, Universitätsmedizin Rostock, Rostock, Mecklenburg-Vorpommern, Germany; Kylie E. Hunter, University of Sydney, Camperdown, New South Wales, Australia; Rebecca K. Golley, Flinders University, Adelaide, South Australia, Australia
.jpg)
Brittany J. Johnson, BND, BHSc(hons), PhD (she/her/hers)
Senior Research Fellow
Flinders University
Bedford Park, South Australia, Australia
Presenting Author(s)
Background: Early childhood obesity prevention initiative that aim to change parent/caregiver practices related to infant (milk) feeding, food provision and parent feeding, movement (including activity, sedentary behaviour) and/or sleep health (i.e. target behaviour clusters) are diverse and heterogeneously reported.
Objective: We aimed to 1) systematically characterise the target behaviours, delivery features, and Behaviour Change Techniques (BCTs) used in interventions in the international TOPCHILD Collaboration, and 2) explore similarities and differences in BCTs used in interventions by target behaviour clusters.
Design/Methods: Systematic searches were performed in 5 databases and 2 clinical trial registries, from inception to February 2023. Trialists from eligible randomised controlled trials of parent-focused, behavioural early obesity prevention interventions shared unpublished intervention materials. Standardised approaches were used to code target behaviours, delivery features and BCTs, using novel approaches of coding unpublished intervention materials and validation meetings with trialist to confirm coding. Narrative syntheses were performed.
Results: 32 trials reporting 37 active intervention arms were included. Interventions targeted a range of behaviours, most frequent combination targeting all behaviour clusters (n=15/37, Fig 1). Delivery features varied greatly. Most interventions were delivered by a health professional (n=26/36), included facilitator training (n=31/36), and were interactive (n=28/36). Overall, 49 of 93 BCTs were coded to at least one target behaviour cluster. The most frequently coded BCTs were: Instruction on how to perform a behaviour (n[arms by cluster]=102), Behavioural practice and rehearsal (n=85), Information about health consequences (n=85), Social support (unspecified) (n=84), and Credible source (n=77). Similar BCTs were often used for each target behaviour cluster.
Conclusion(s): Our study provides the most comprehensive description of the behaviour change content of complex interventions targeting early childhood obesity prevention. Our analysis revealed interventions targeted multiple behaviour clusters, with significant variation in delivery features. Despite the diverse range of BCTs coded, five BCTs were consistently identified across clusters, though certain BCTs were more prevalent in specific clusters. These findings can inform design of future interventions to draw on commonly used components in existing interventions and gaps in underused intervention components.
Figure 1: Frequency of combinations of target parental behaviour clusters coded in early child obesity prevention interventions (N=37)a
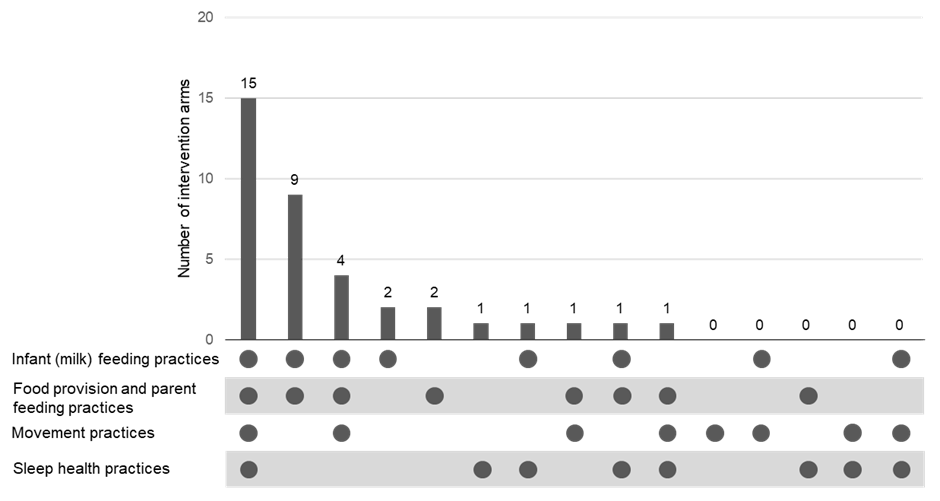 a The x-axis details the possible combinations of the four target parental behaviour clusters, with the dots indicating cluster present in that combination. The y-axis indicates the number of interventions that targeted that combination of clusters. Zeros represent that no intervention targeted the combination of clusters.
a The x-axis details the possible combinations of the four target parental behaviour clusters, with the dots indicating cluster present in that combination. The y-axis indicates the number of interventions that targeted that combination of clusters. Zeros represent that no intervention targeted the combination of clusters.
